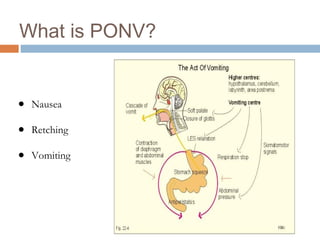
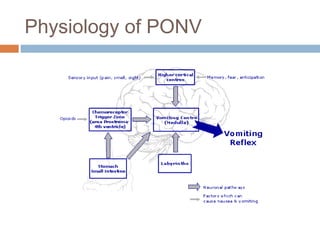
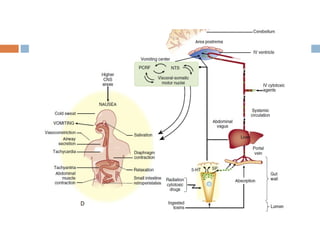
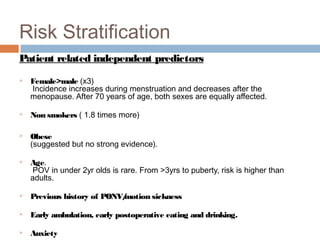
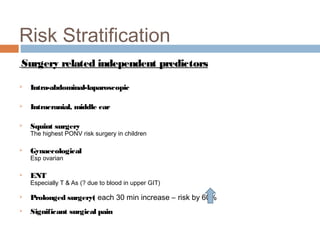
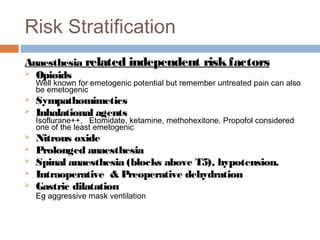
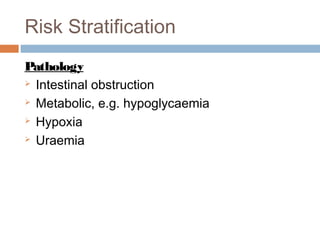
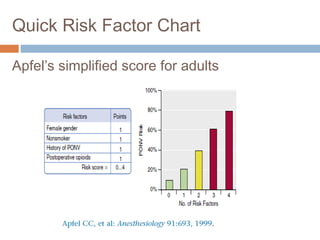
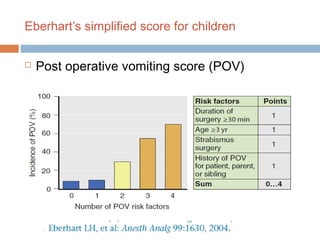
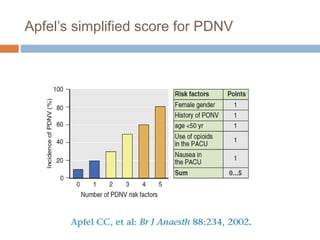
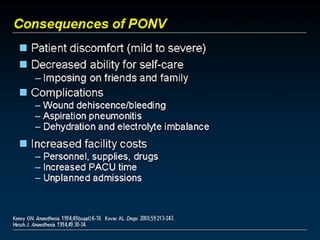
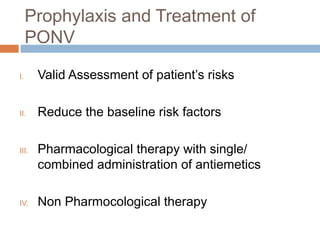
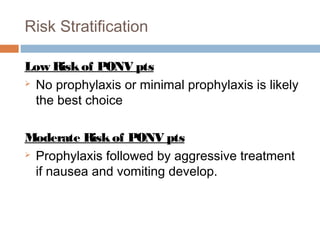
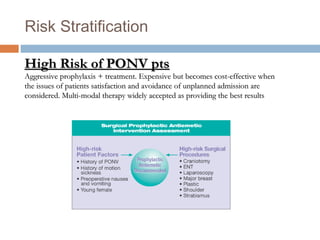
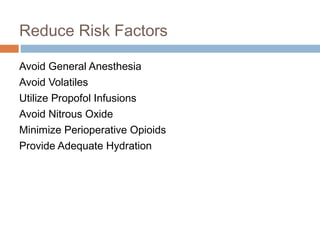
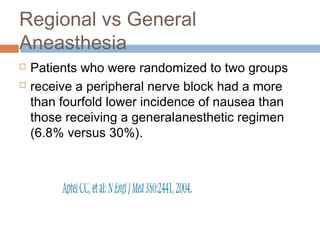
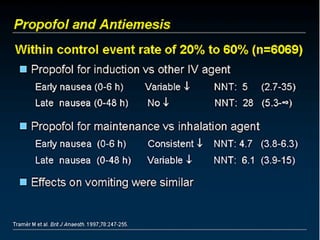
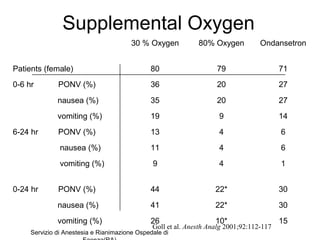
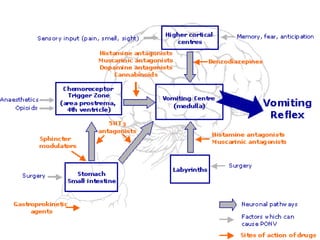
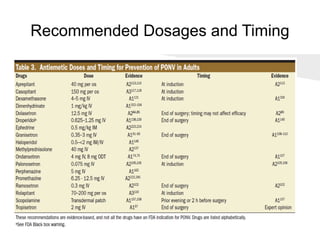
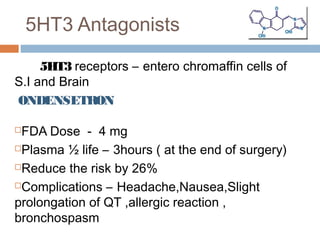
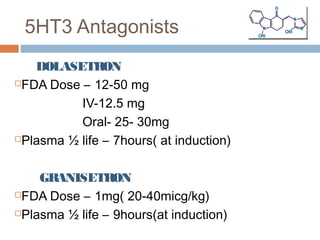
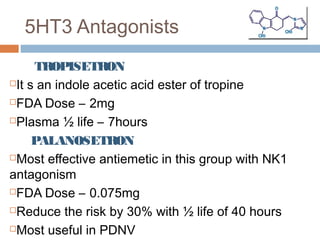
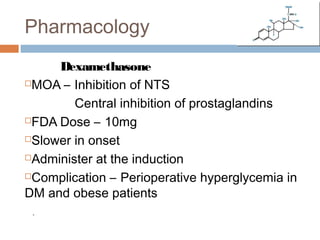
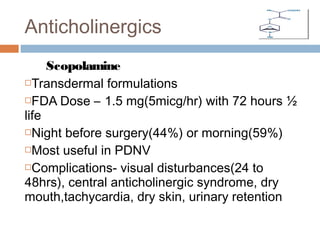
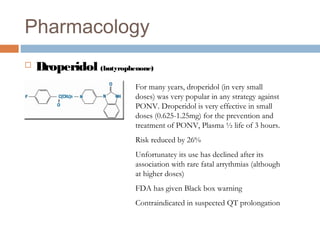
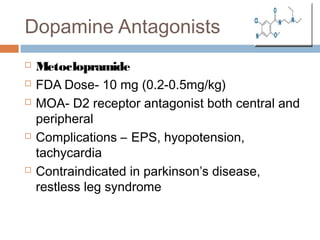
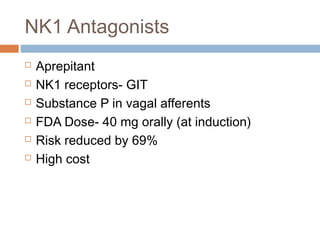
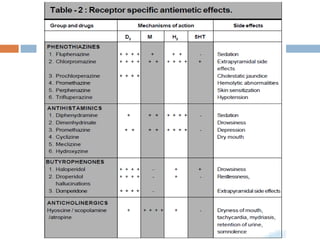
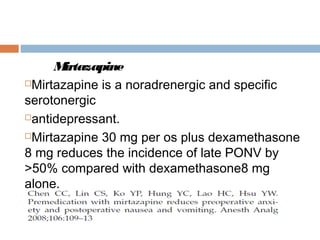
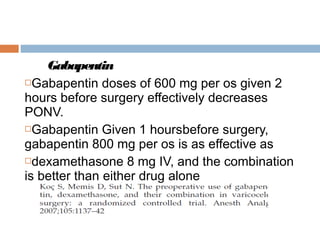
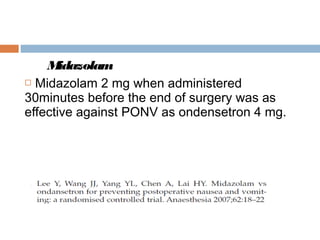
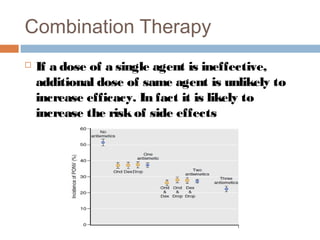
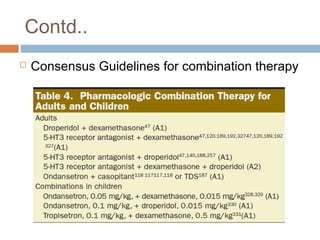
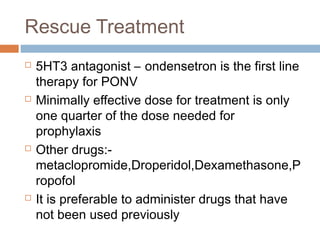
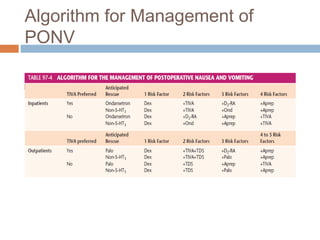
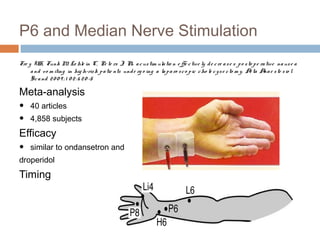
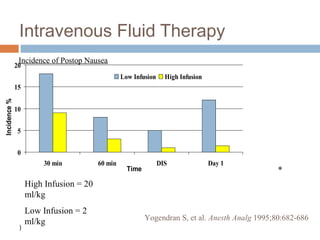
This document discusses postoperative nausea and vomiting (PONV). It begins by explaining why PONV is an important issue, noting the high incidence rates and negative patient experiences and outcomes associated with it. It then covers the physiology and classification of PONV. Major sections discuss risk stratification and identification of independent risk factors, as well as pharmacological and non-pharmacological prophylaxis and treatment options. Drug therapies covered include 5-HT3 receptor antagonists, NK-1 receptor antagonists, corticosteroids, butyrophenones, and other classes. Non-drug approaches like acupuncture, hydration, and hypnosis are also mentioned.