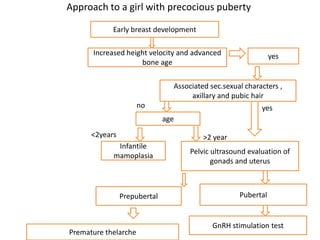
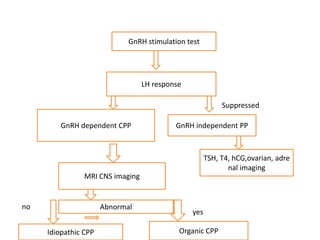
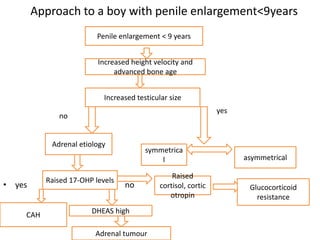
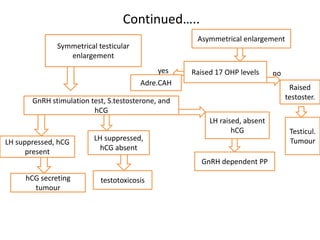
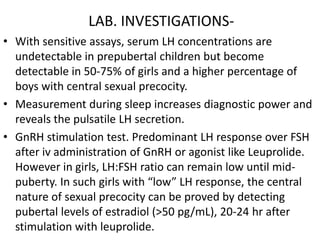
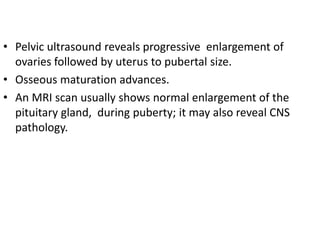
The document discusses precocious puberty, defined as the onset of secondary sexual characteristics before age 8 in girls and age 9 in boys, and classifies it into central (gonadotropin-dependent) and peripheral (gonadotropin-independent) types. It details the causes, clinical features, and potential consequences on growth, along with various diagnostic and treatment approaches. The document also covers related conditions, laboratory investigations, and management strategies for both types of precocious puberty in boys and girls.

![TREATMENT-
• Long term GnRH agonists In the USA, the most commonly
used preparation is leuprolide acetate (Lupron Depot Ped),
in a dose of 0.25-0.3 mg/kg (minimum, 7.5 mg) i.m. once
every 4 wk. Other preparations (D-Trp6-GnRH [Decapeptyl],
goserelin acetate [Zoladex]) are approved for treatment of
precocious puberty in other countries.
• Alternatively, histrelin (Supprelin LA), a subcutaneous 50
mg implant with effects lasting 12 mo, is approved by the
FDA .
• Intranasal and subcutaneous injection formulae are also
available.
• IUGR at greater risk of short stature as adults and require
more-aggressive treatment of precocious puberty, possibly
in conjunction with human growth hormone (hGH) therapy.](https://image.slidesharecdn.com/precociouspuberty-130120062118-phpapp02/85/Precocious-puberty-11-320.jpg)

![MAC CUNE ALBRIGHT SYNDROME-
• A rare disorder prevalence 1 in 100000 to 1000000. Is
associated with patchy cutaneous pigmentation and fibrous
dysplasia of the skeletal system.
• a missense mutation in the gene encoding the α-subunit of
GS, the G protein that stimulates cAMP formation, resulting
in the formation of the putative gsp oncoprotein. Activation
of receptors (corticotropin [ACTH], TSH, FSH, and LH
receptors) that operate via a cAMP-dependent
mechanism, as well as cell proliferation, ensue.
• expressed differently in different tissues, accounts for
variability of clinical expression.](https://image.slidesharecdn.com/precociouspuberty-130120062118-phpapp02/85/Precocious-puberty-14-320.jpg)