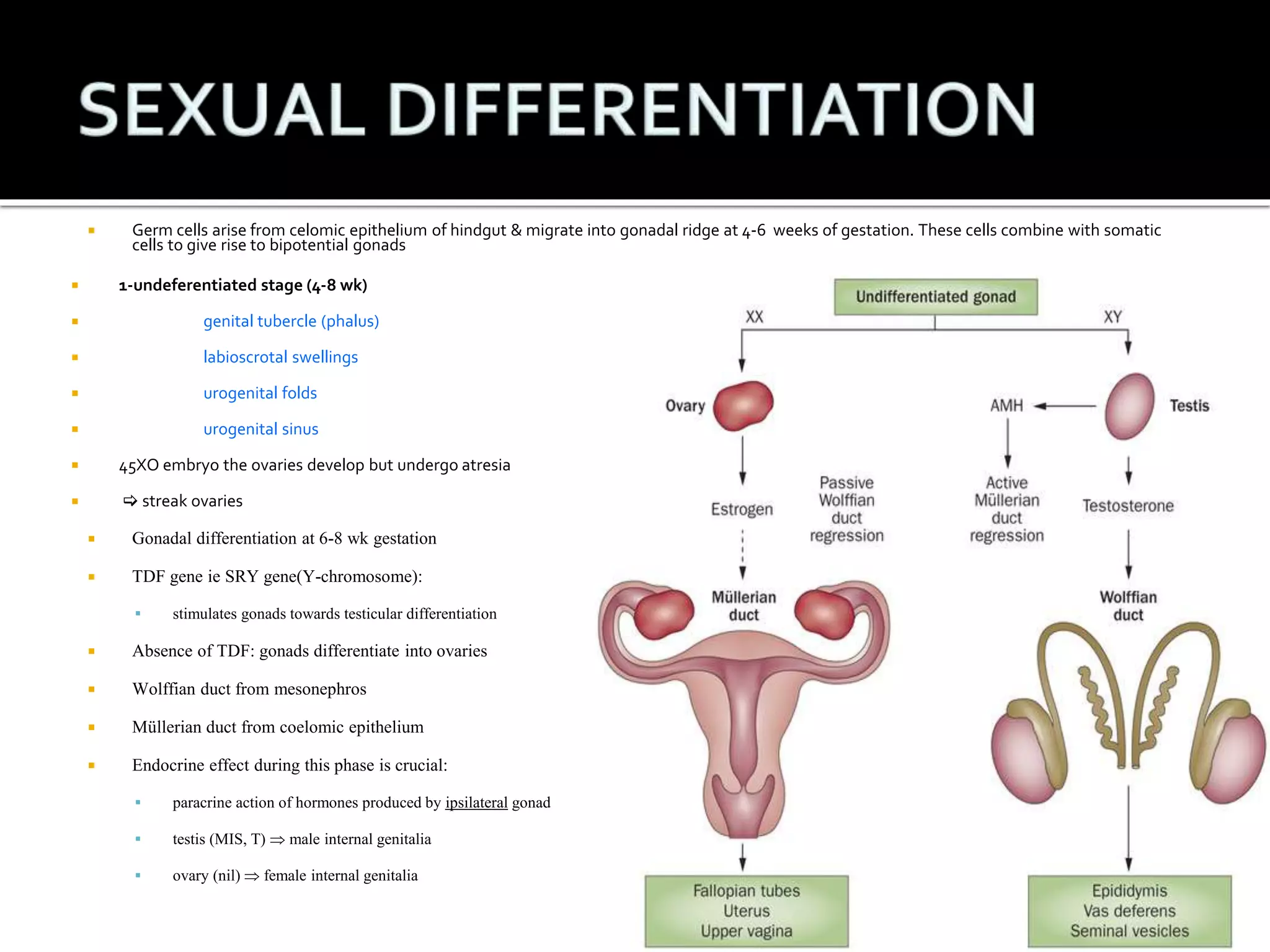
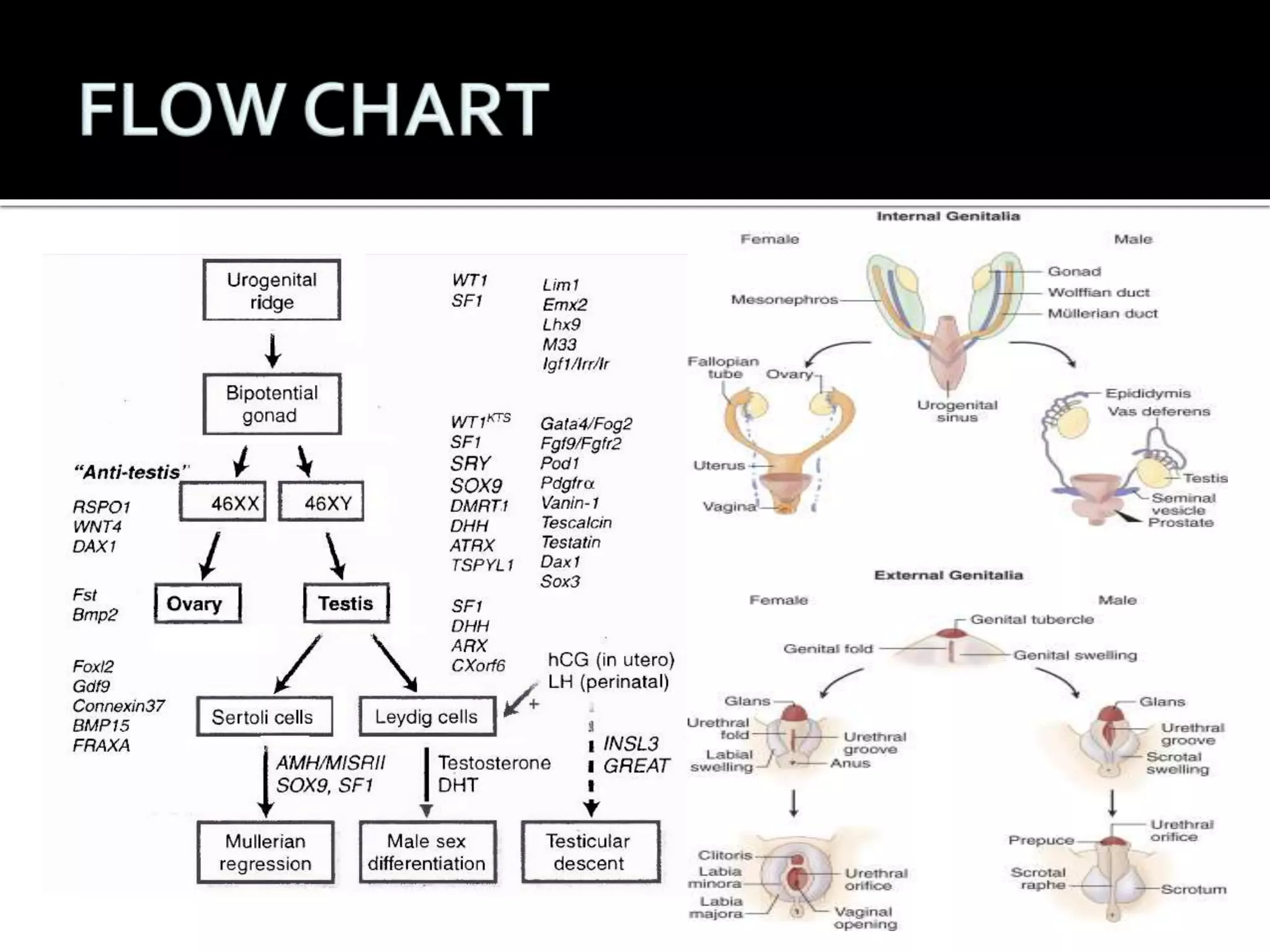
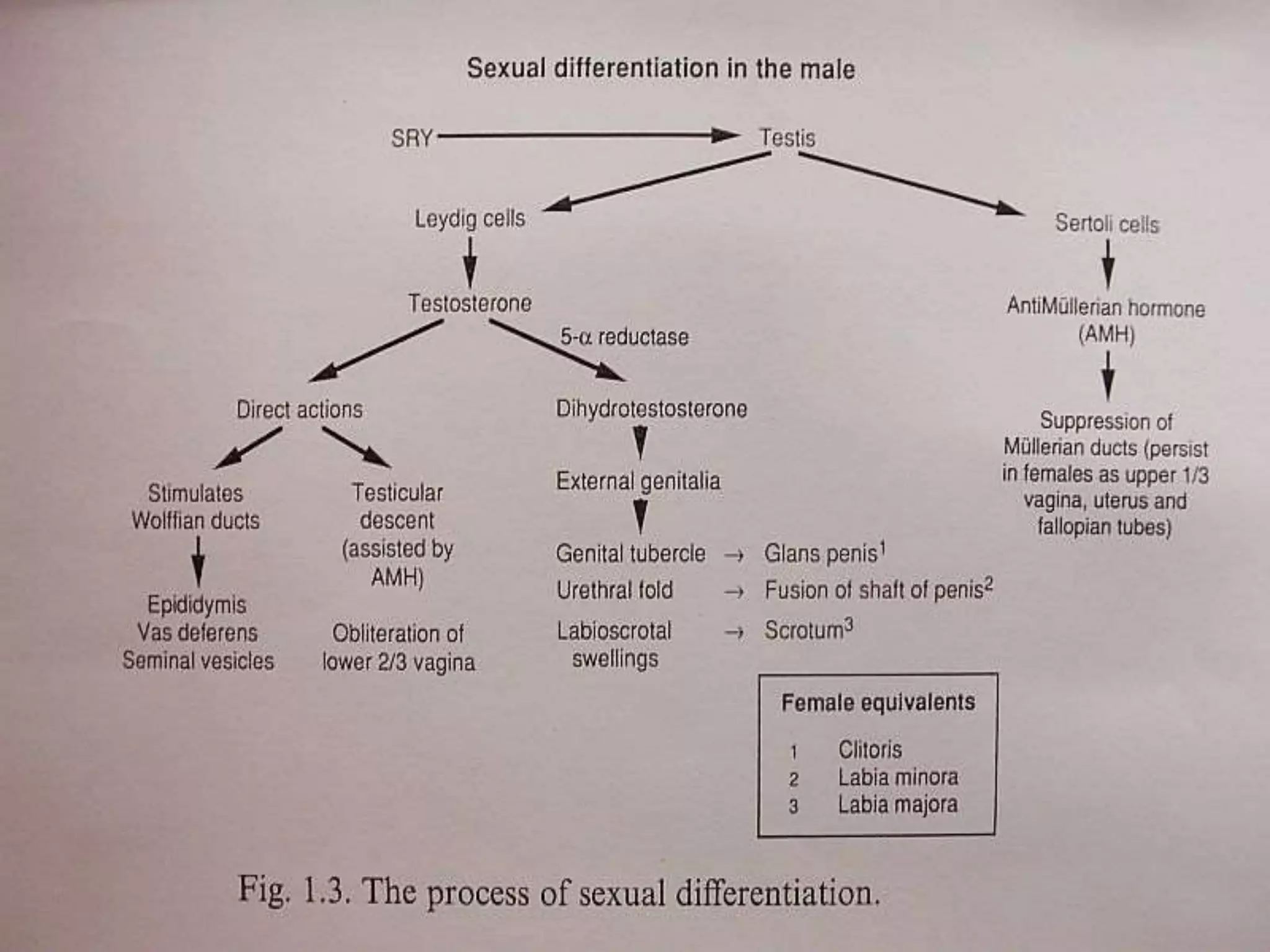
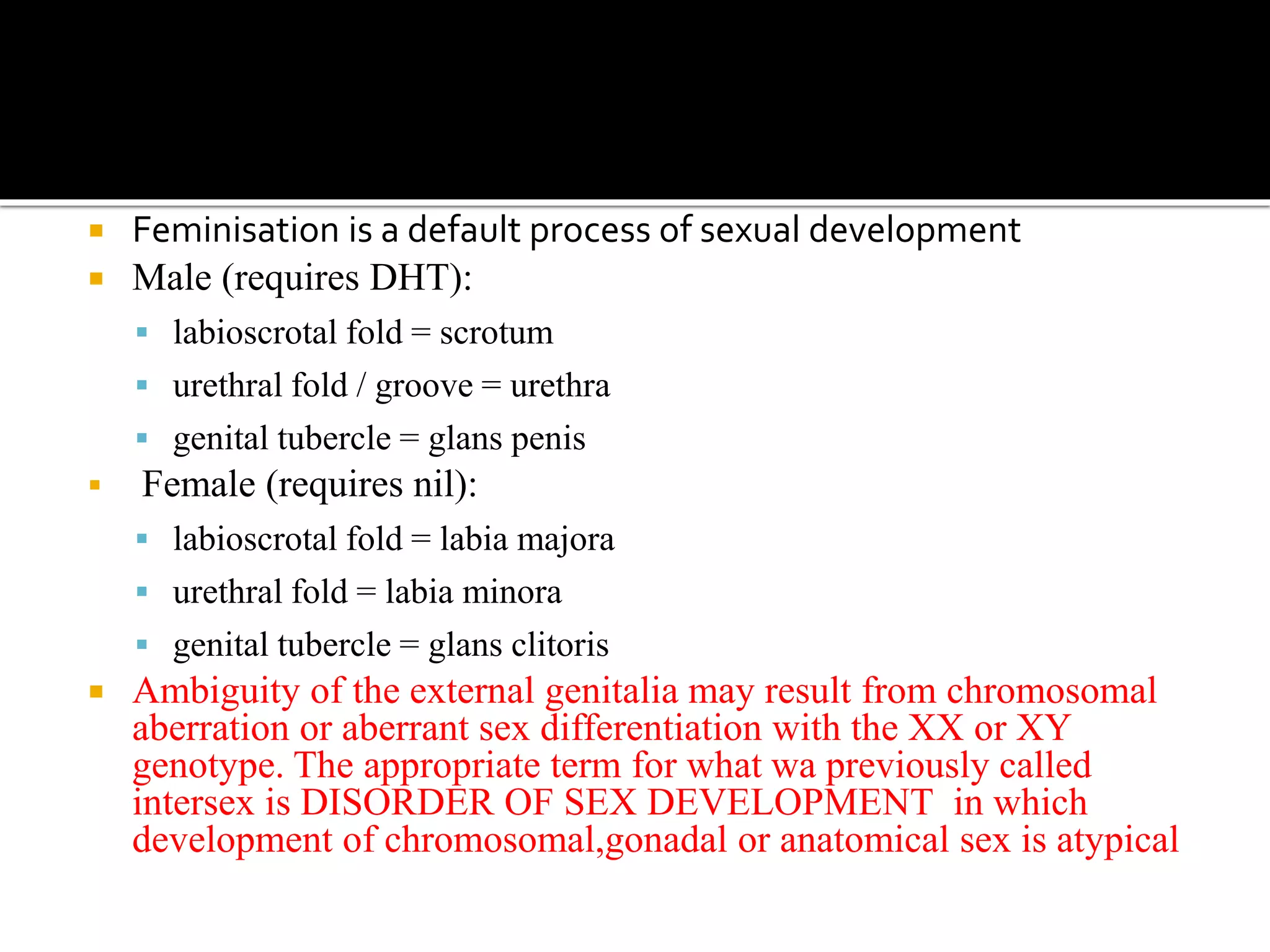
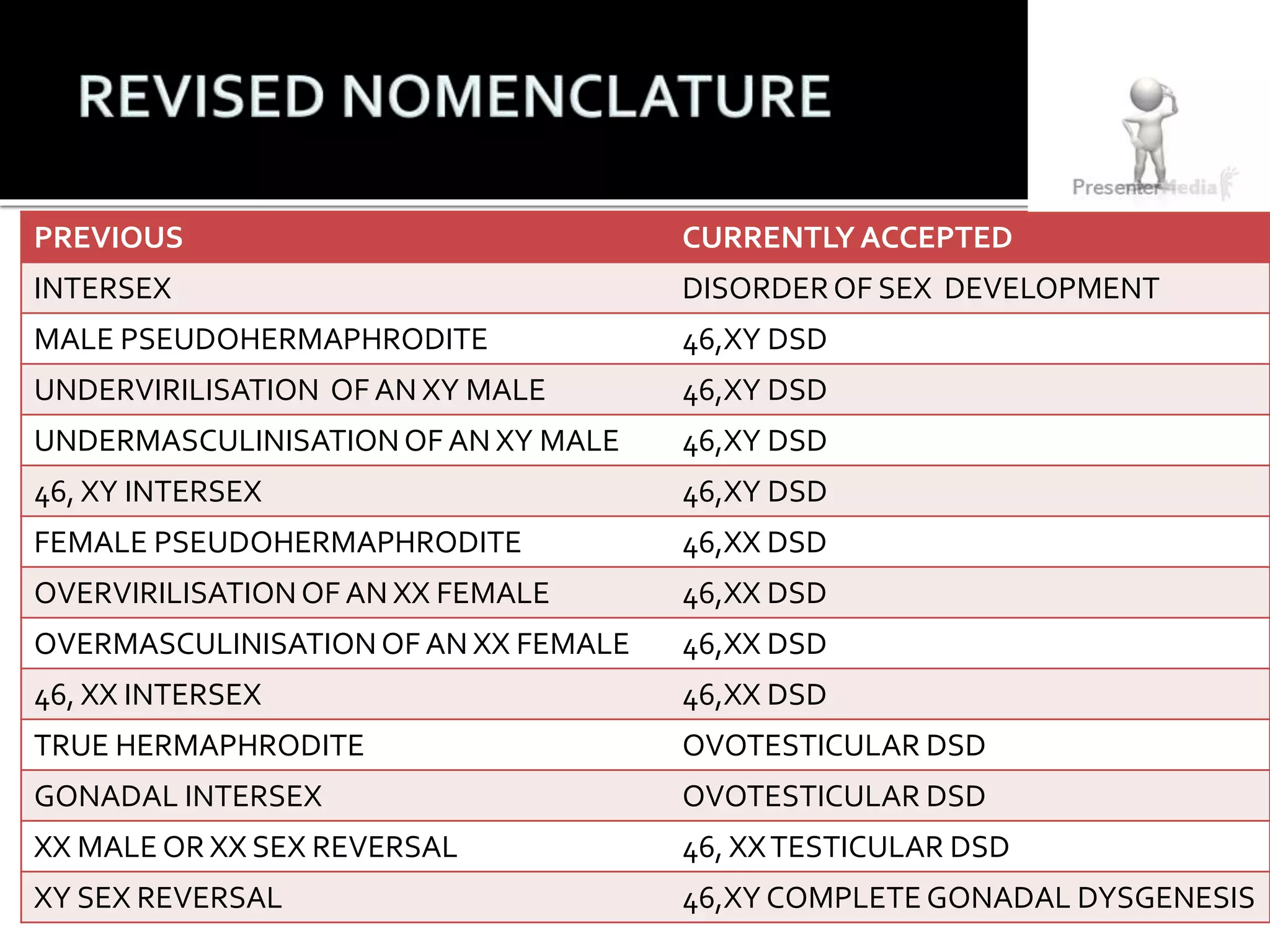
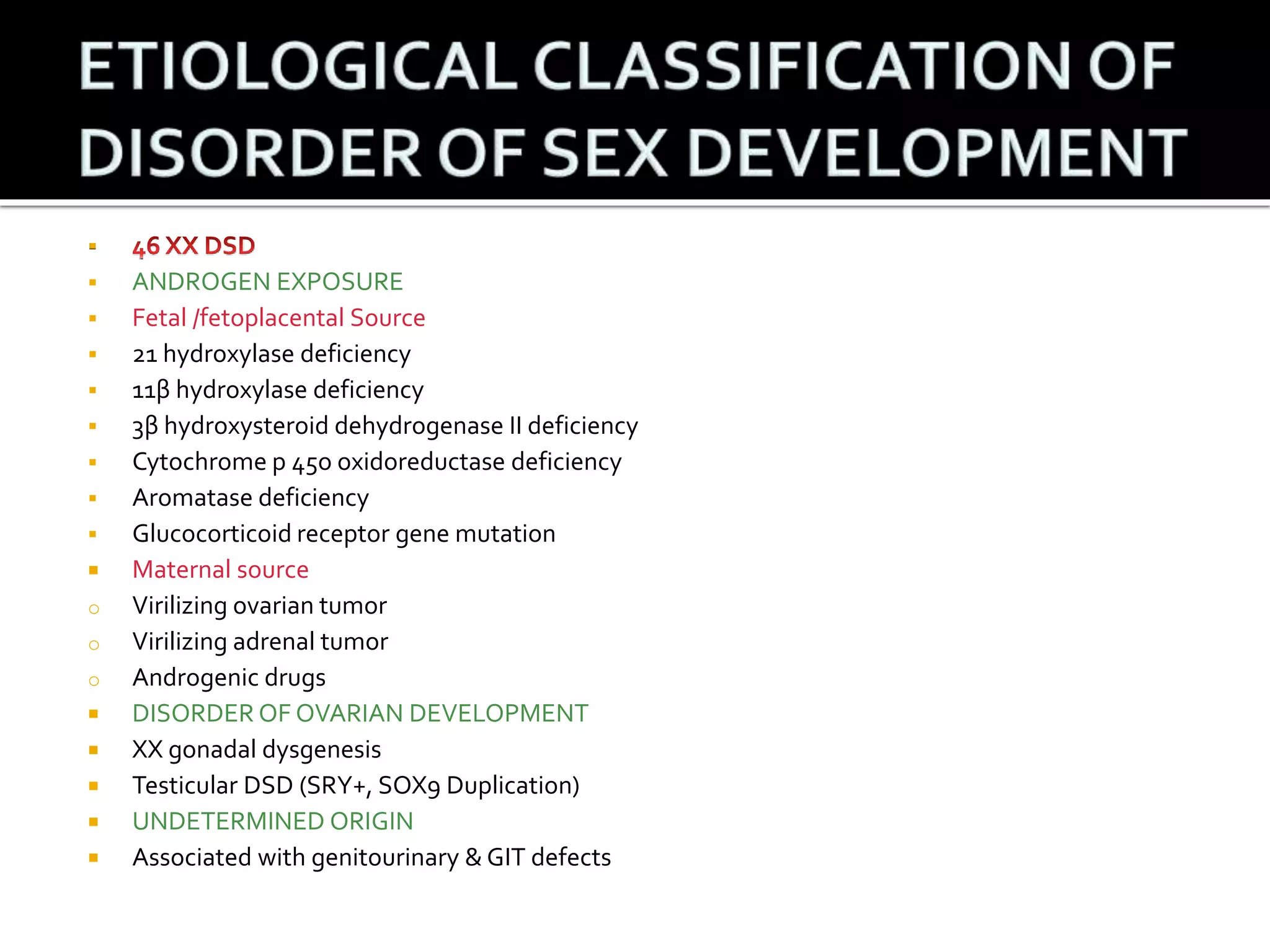
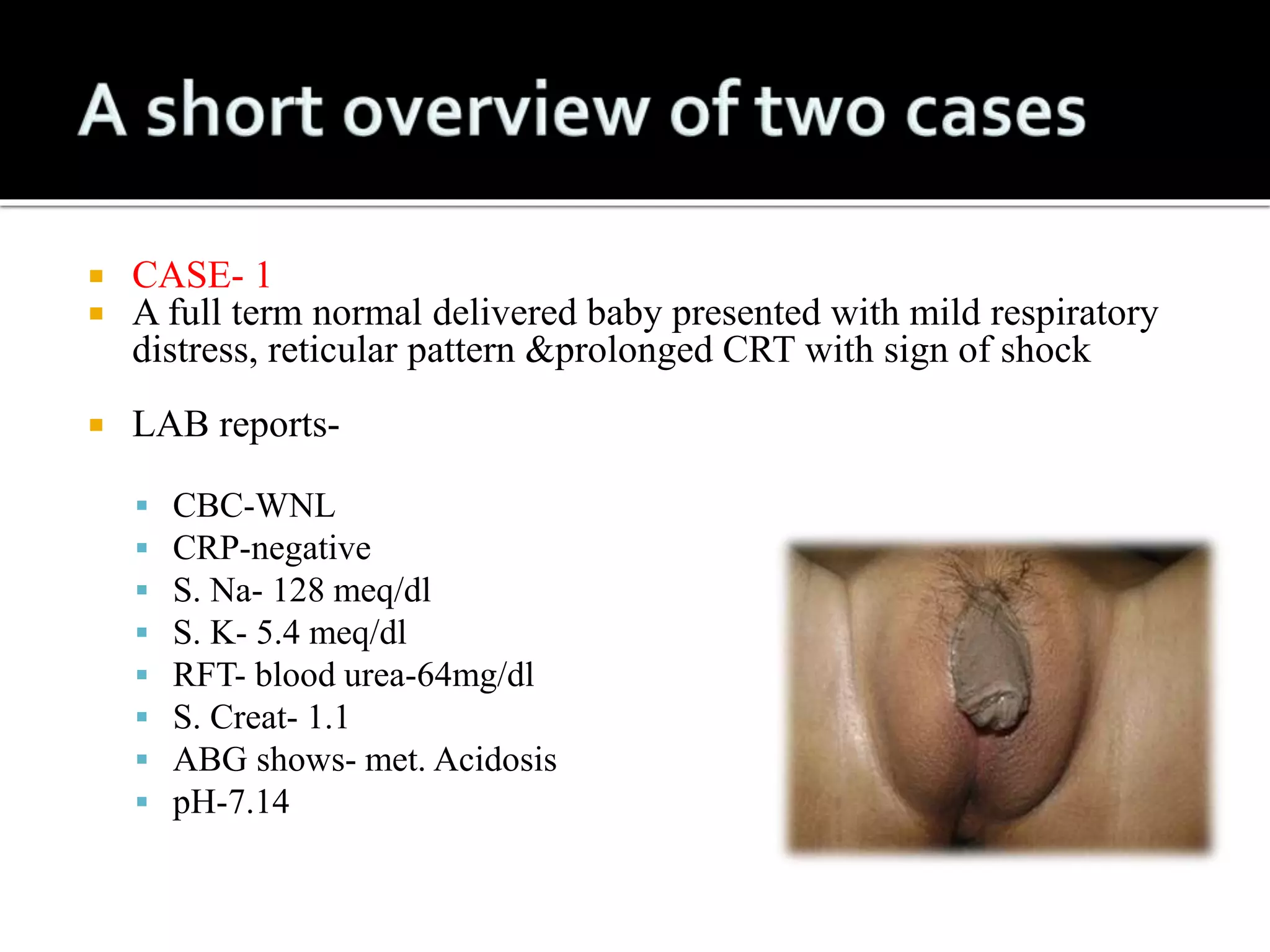
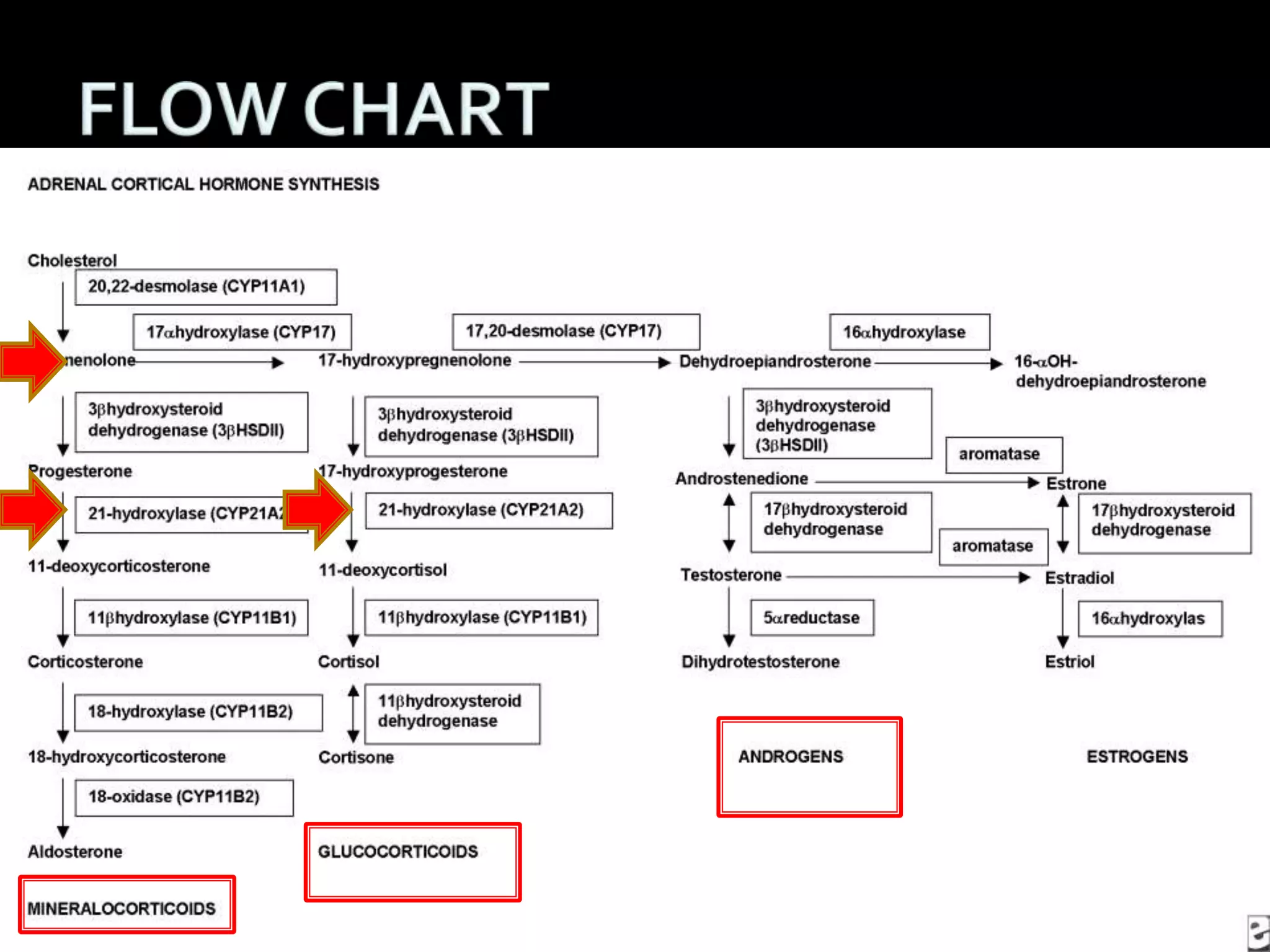
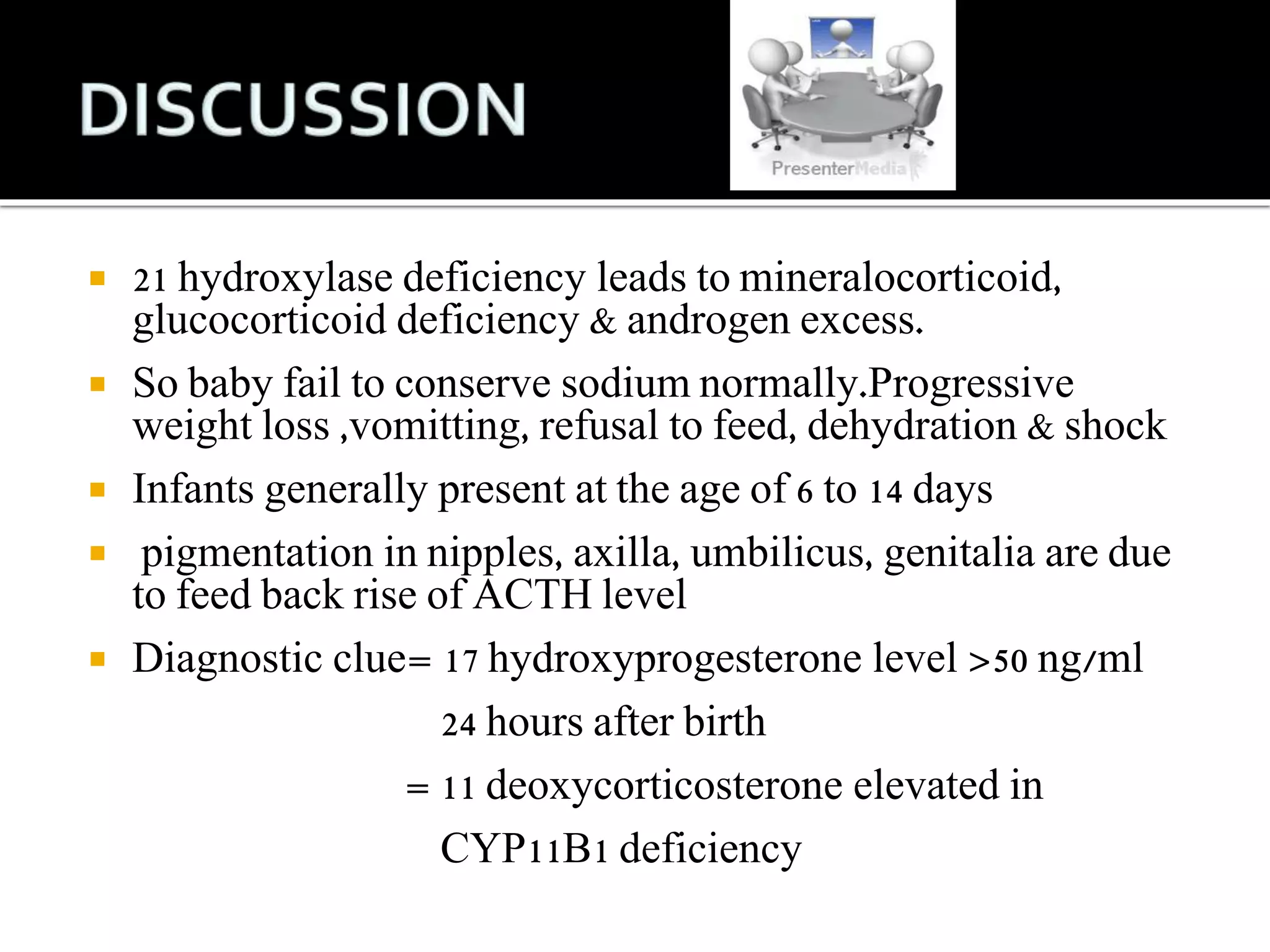
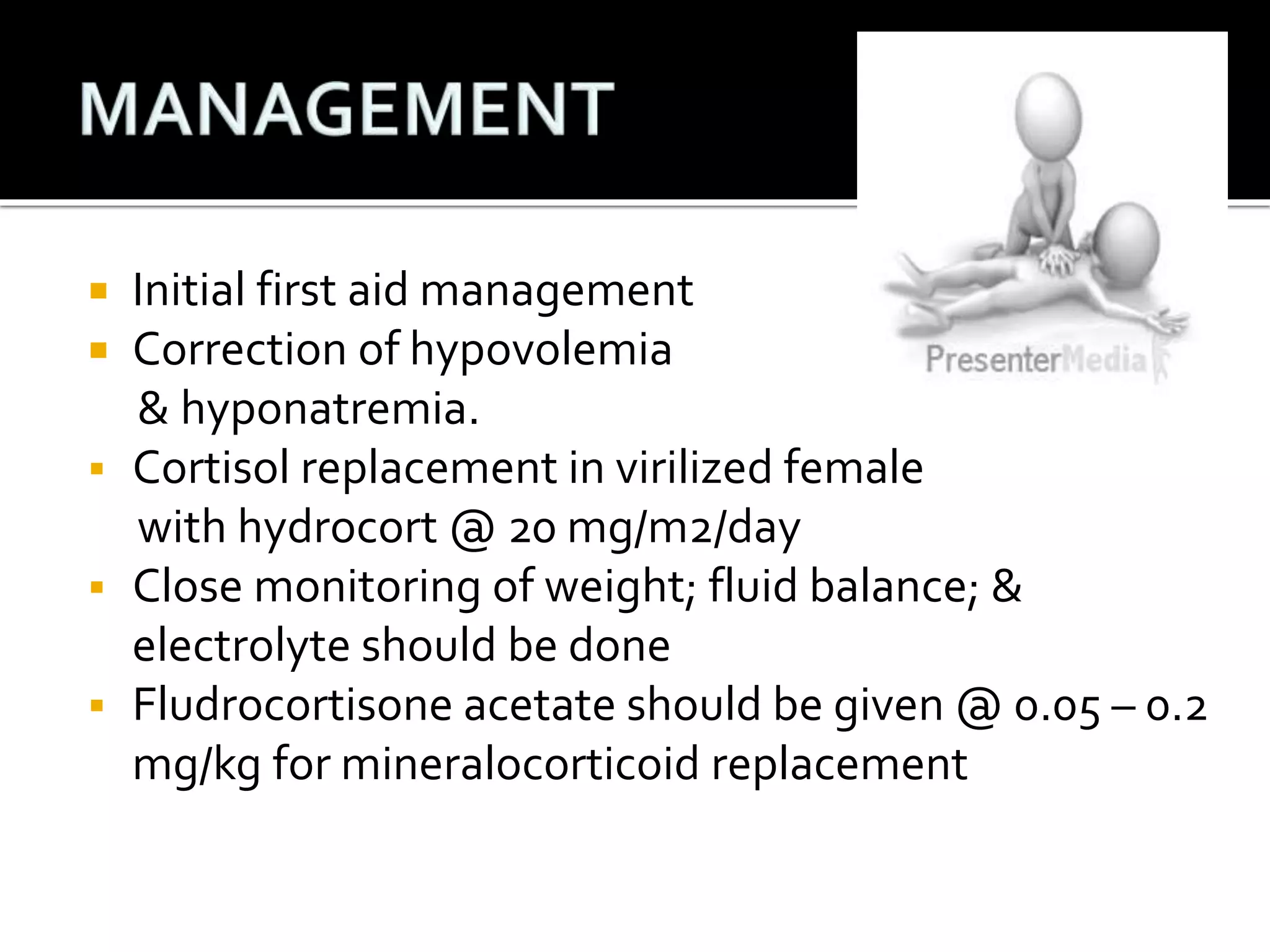
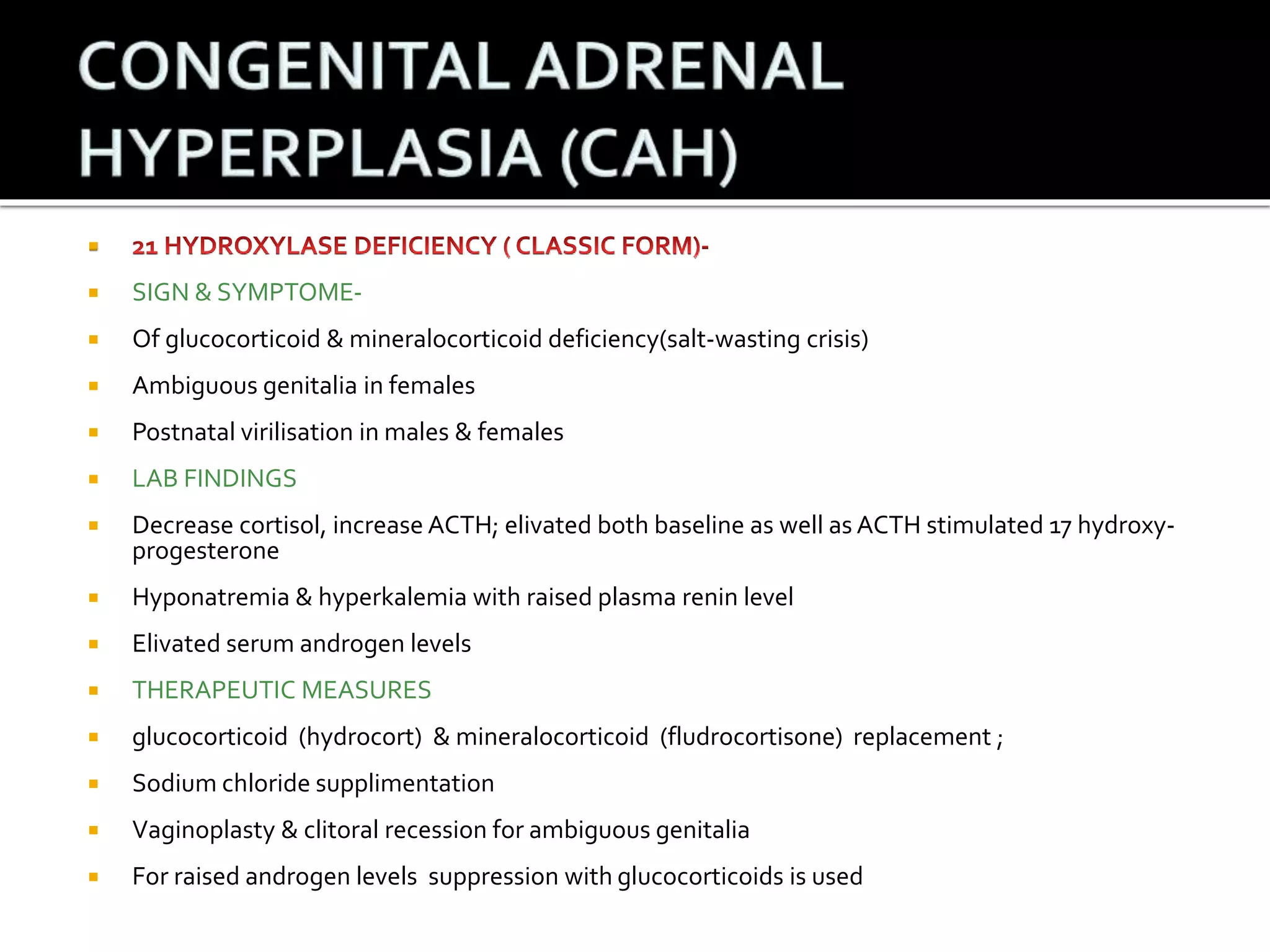
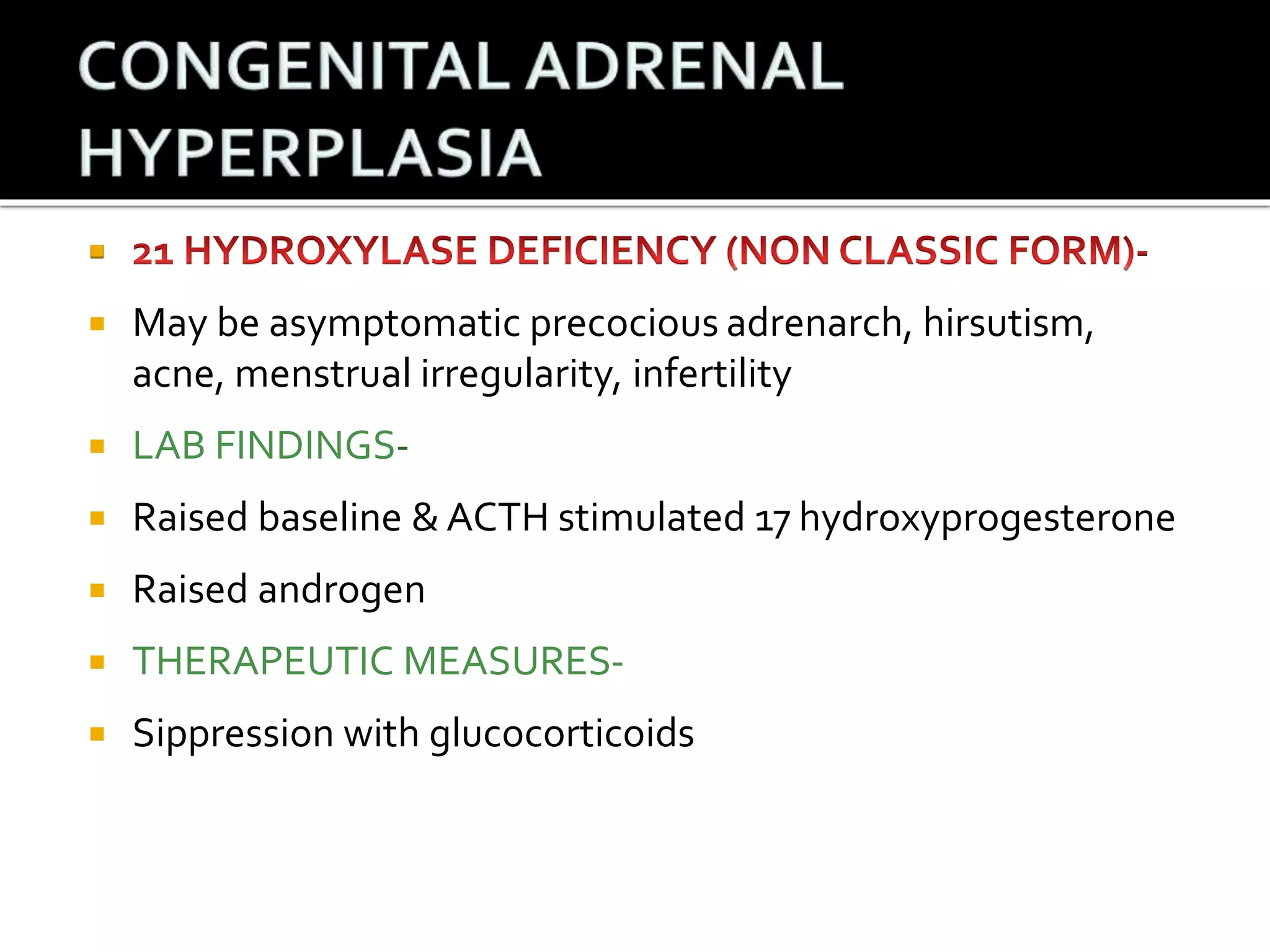
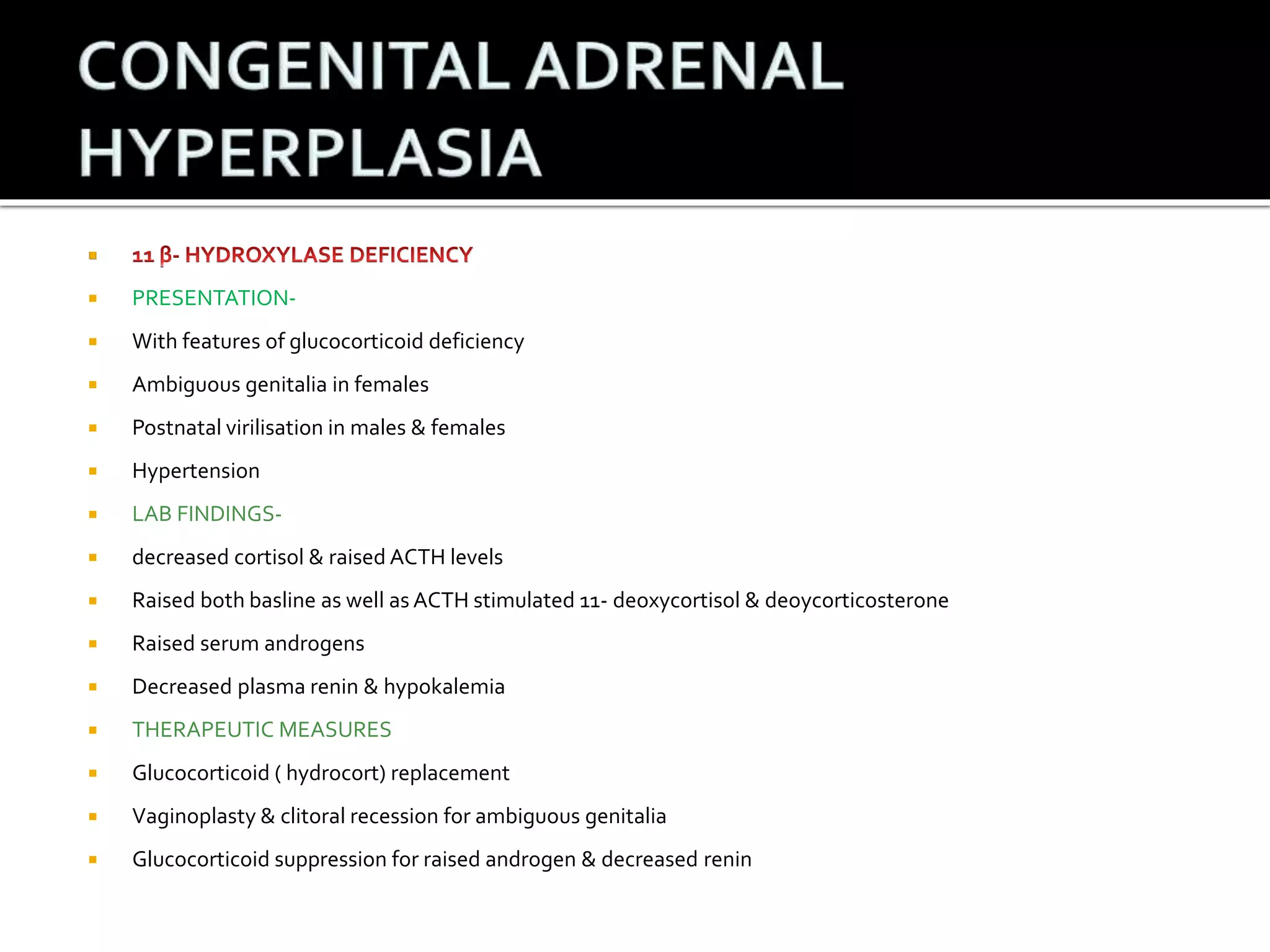
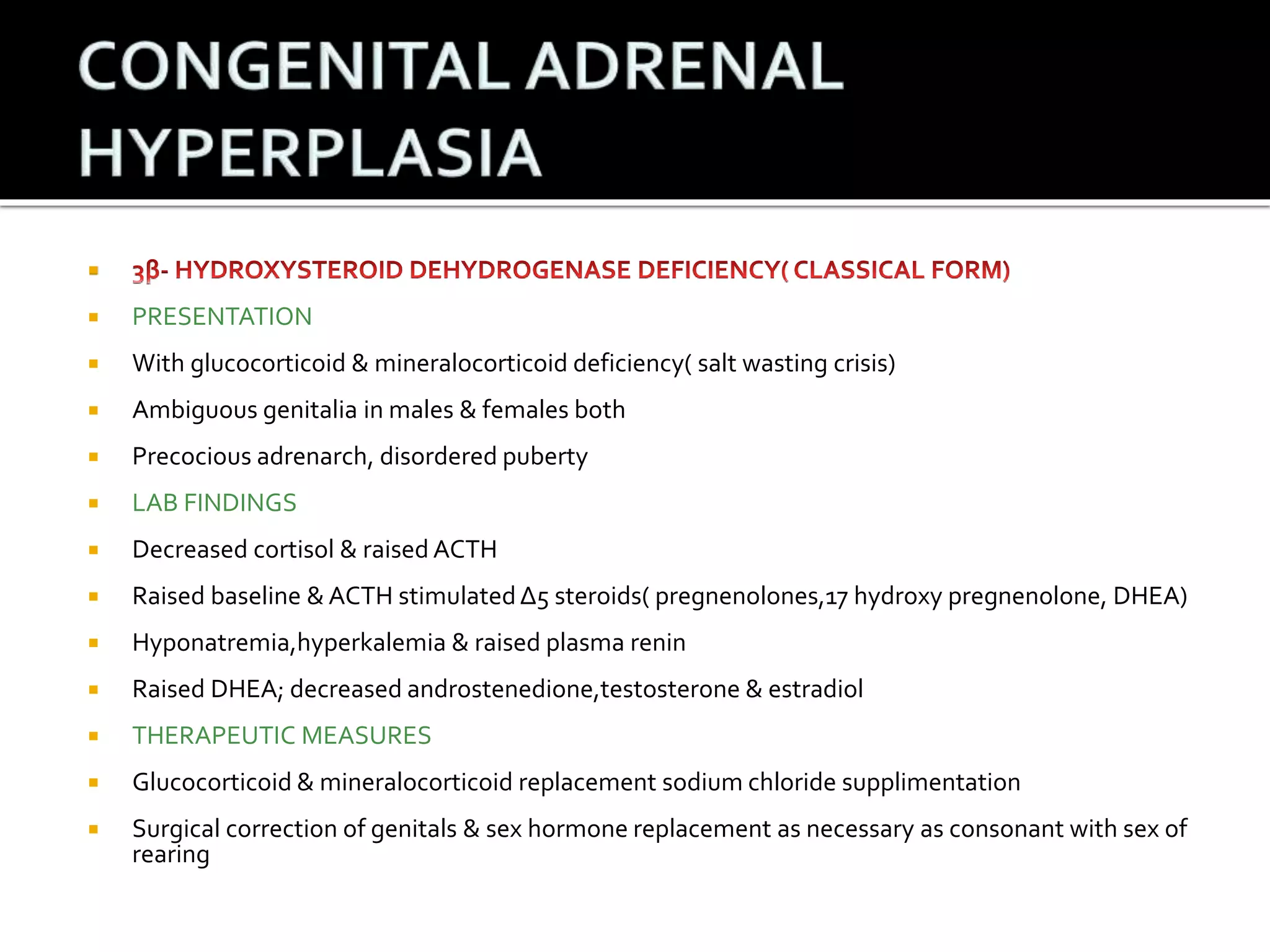
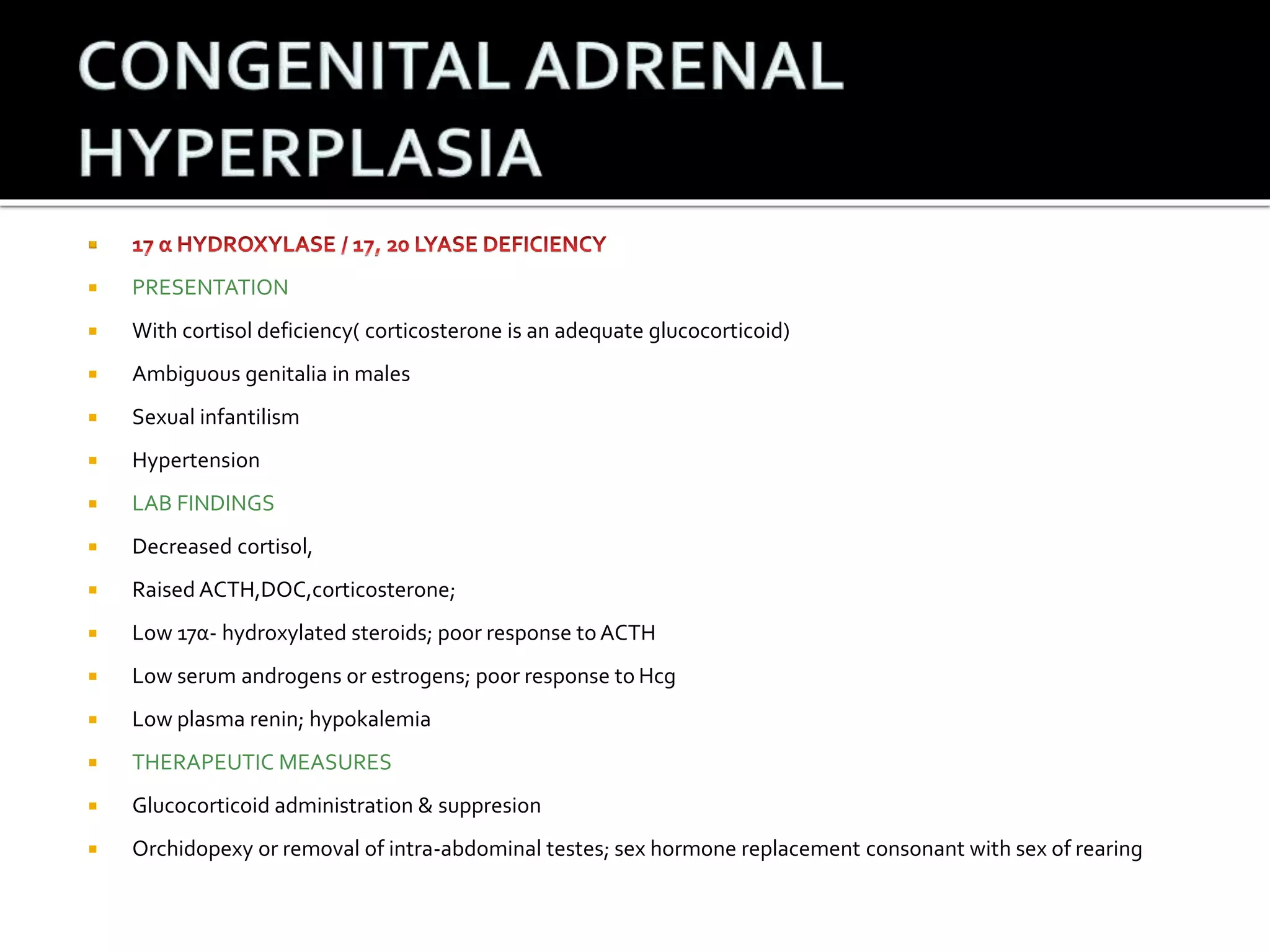
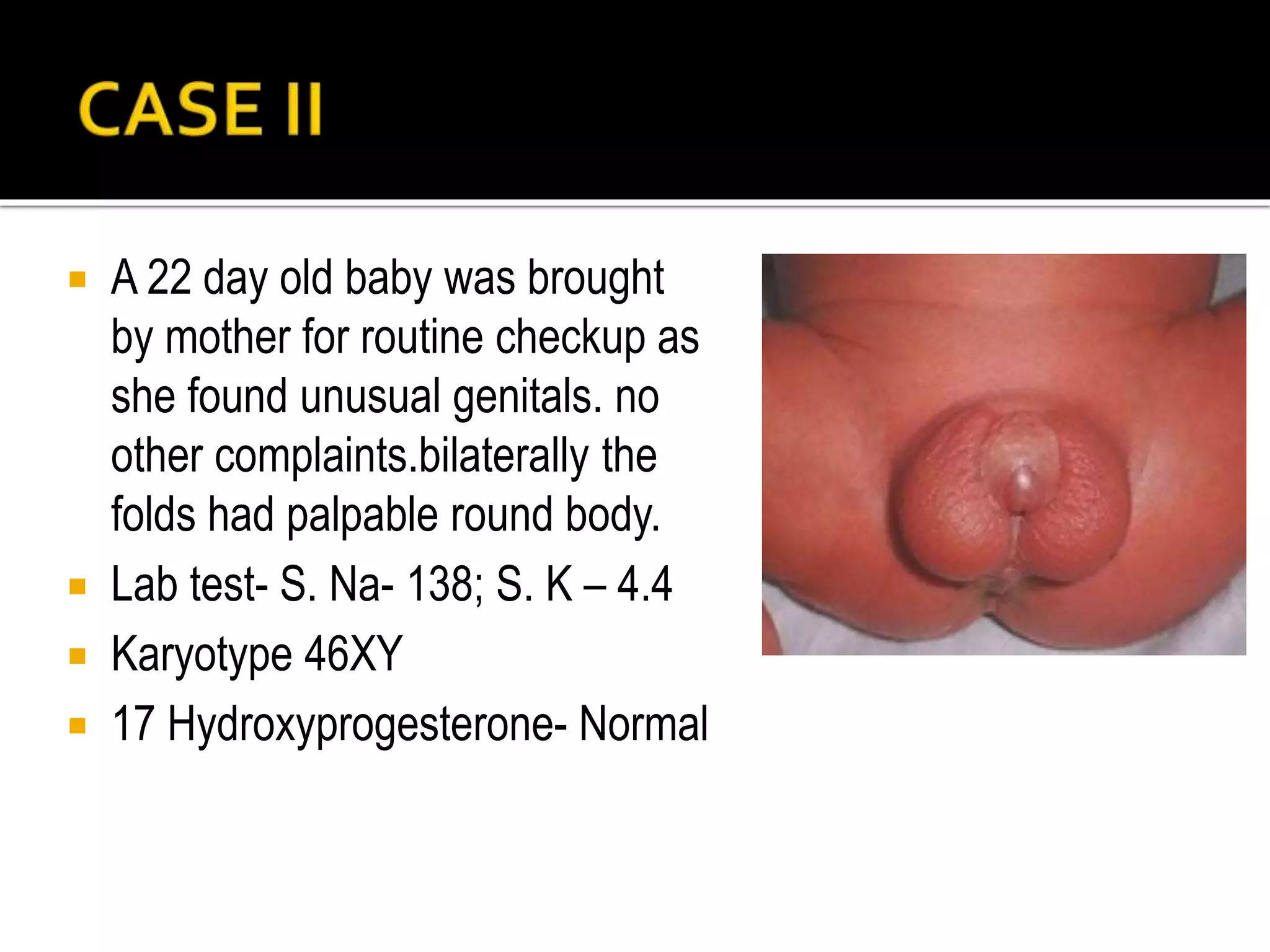
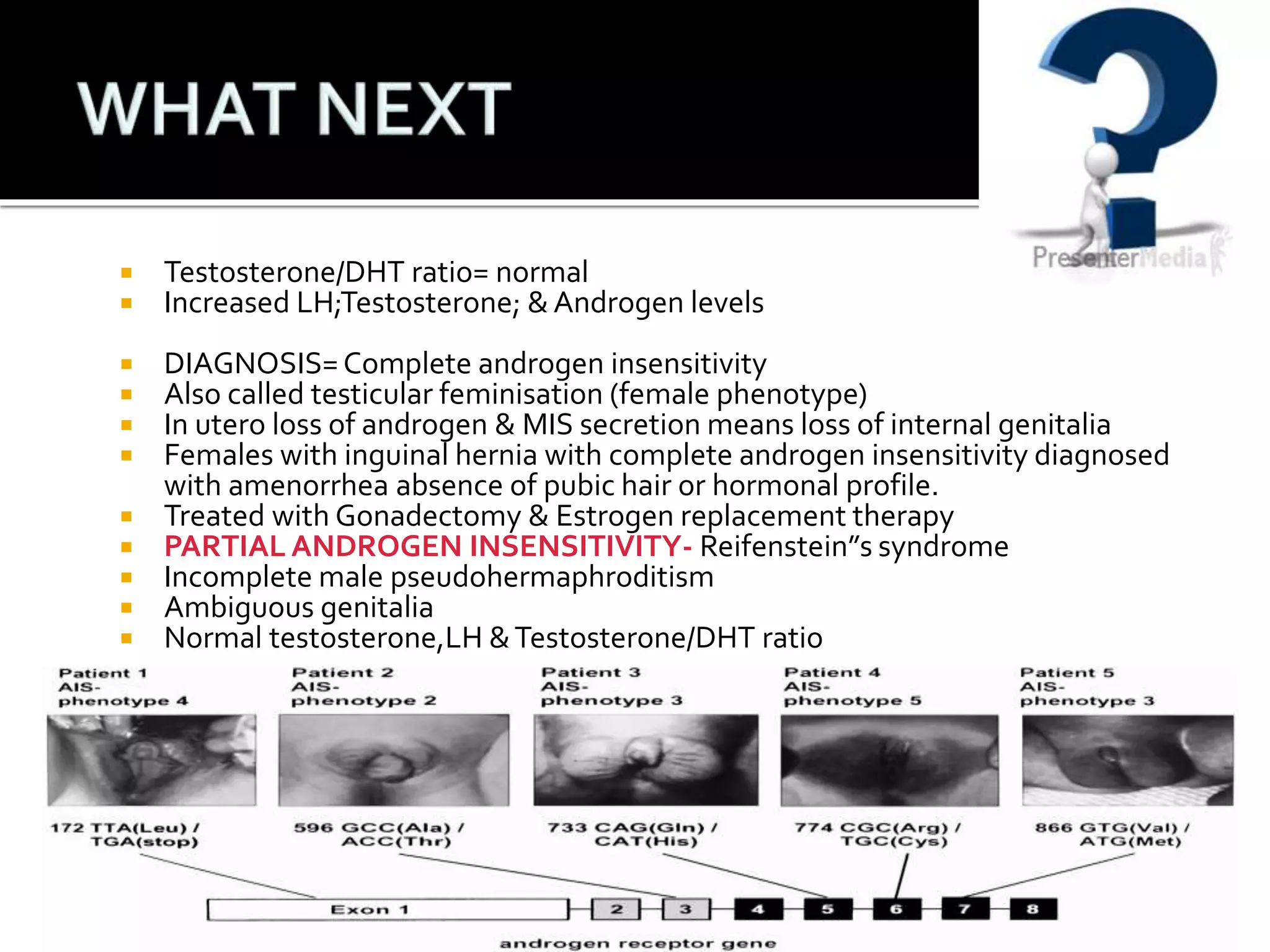
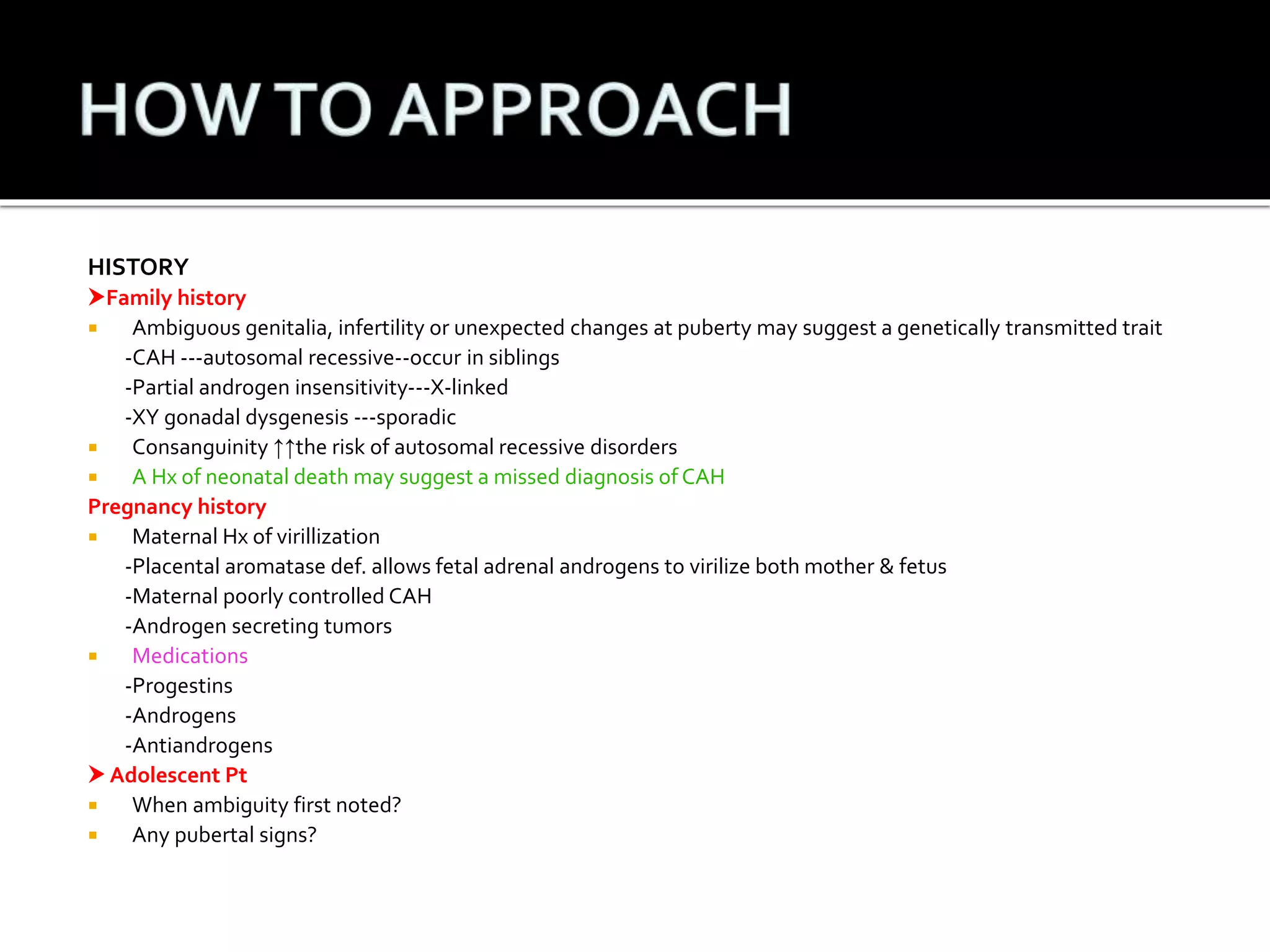
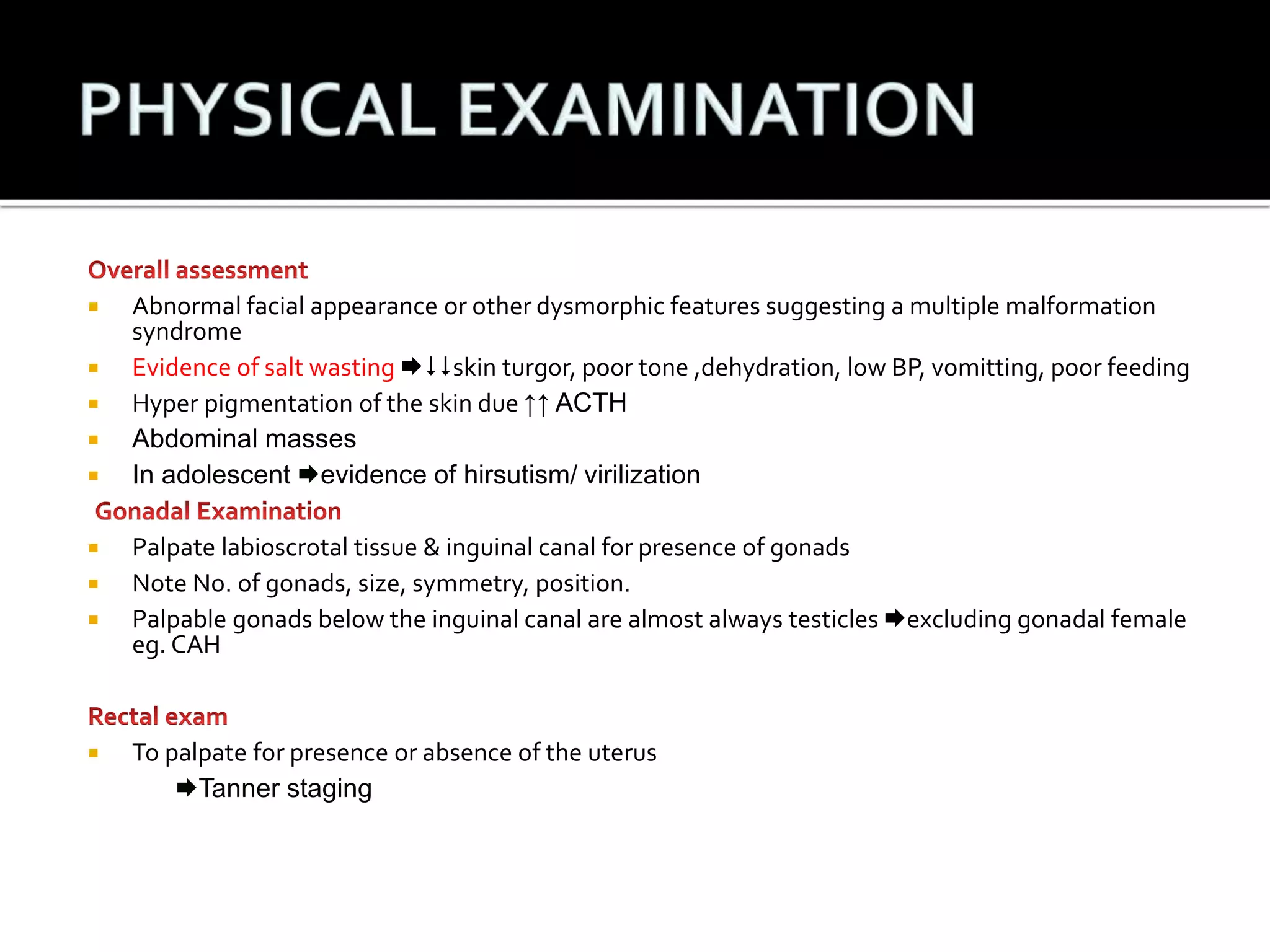
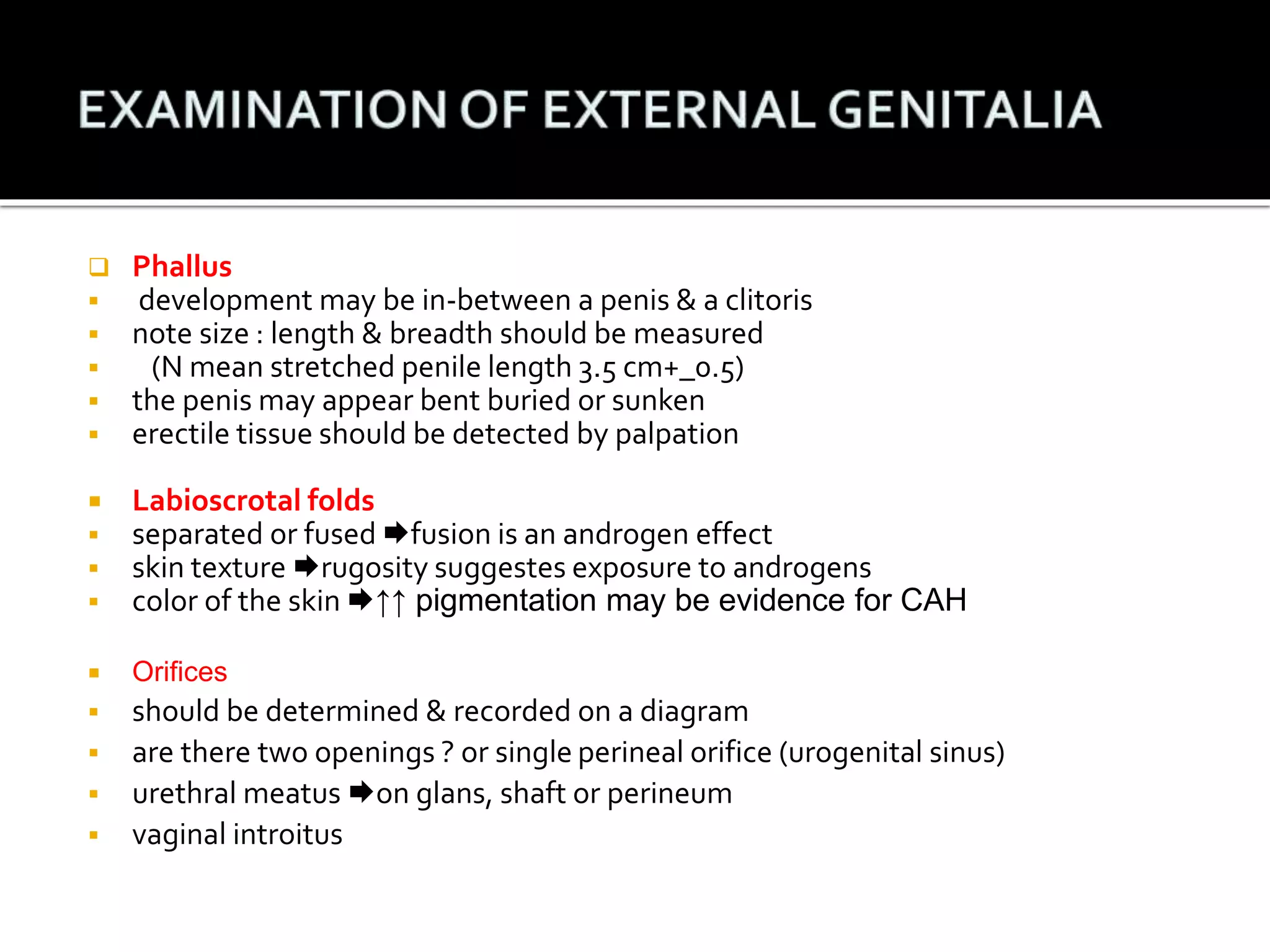
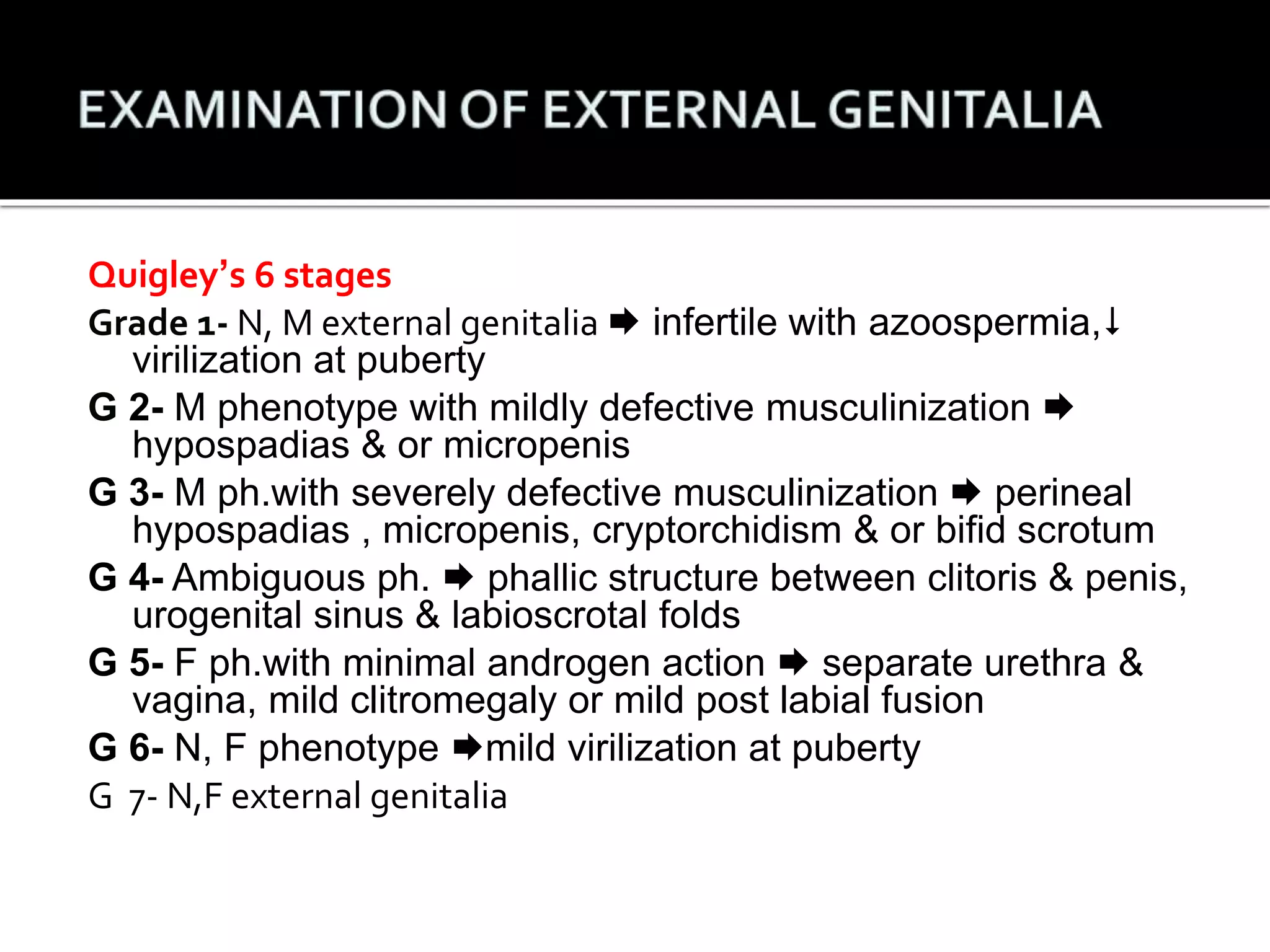
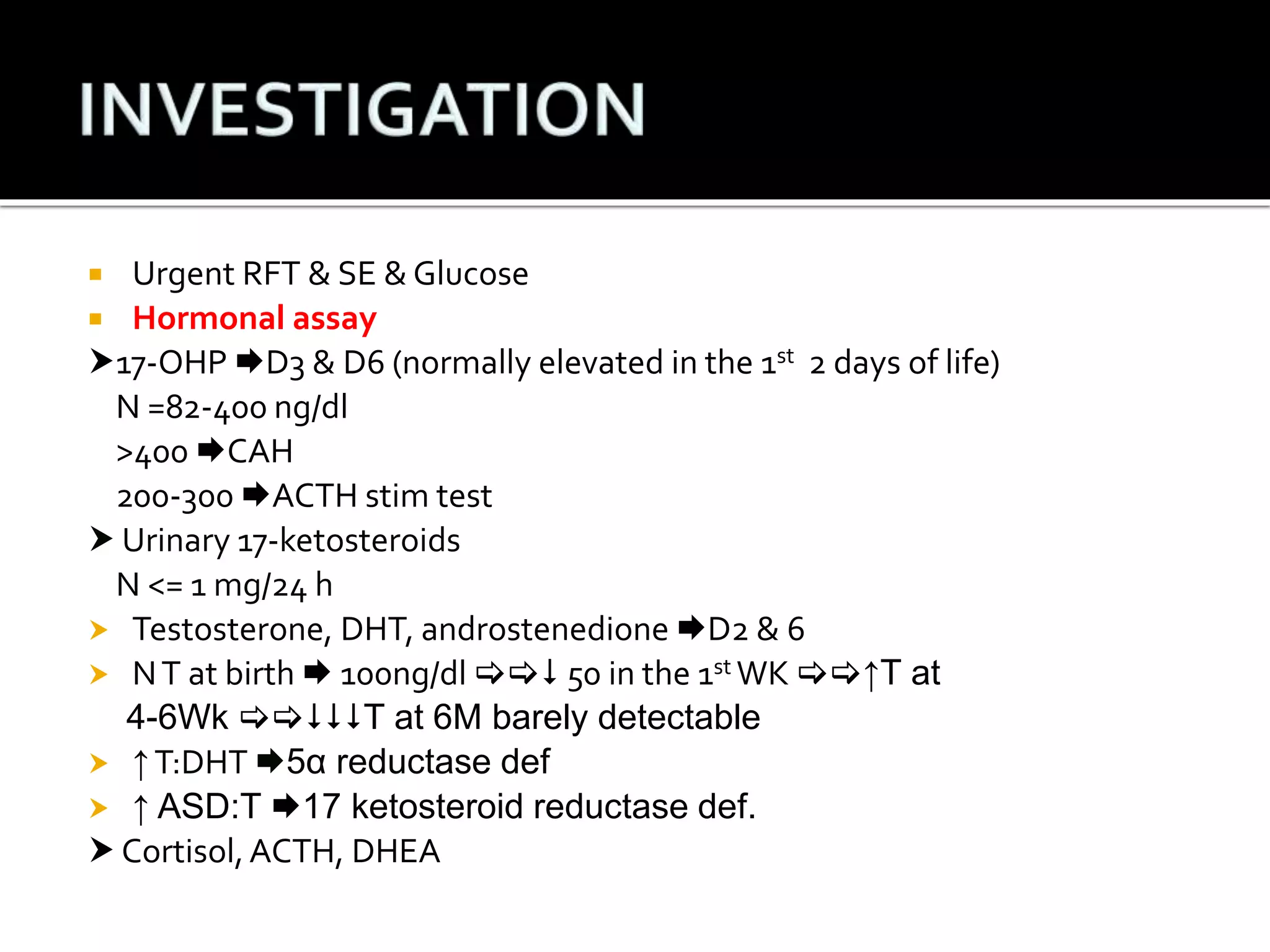
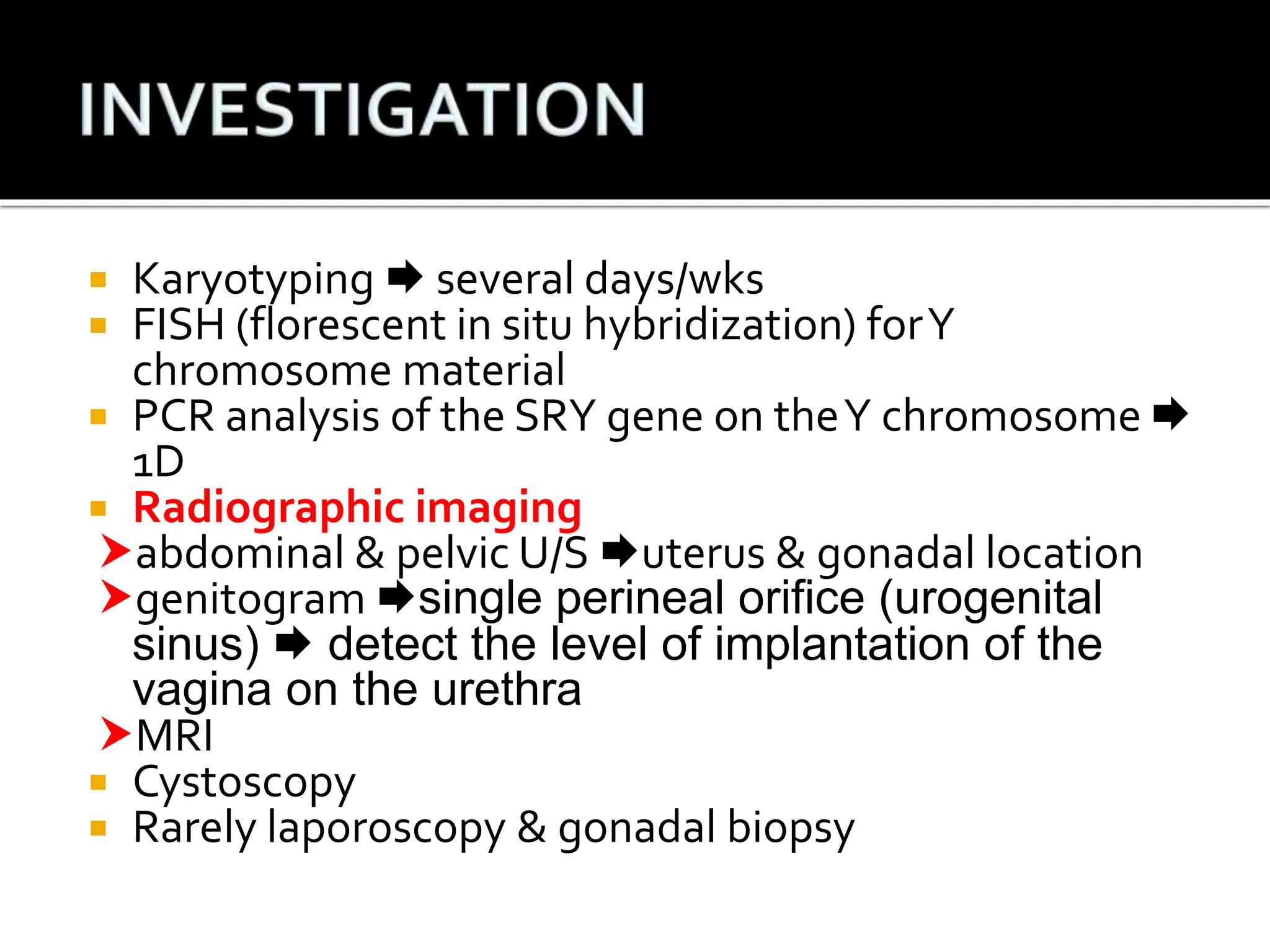
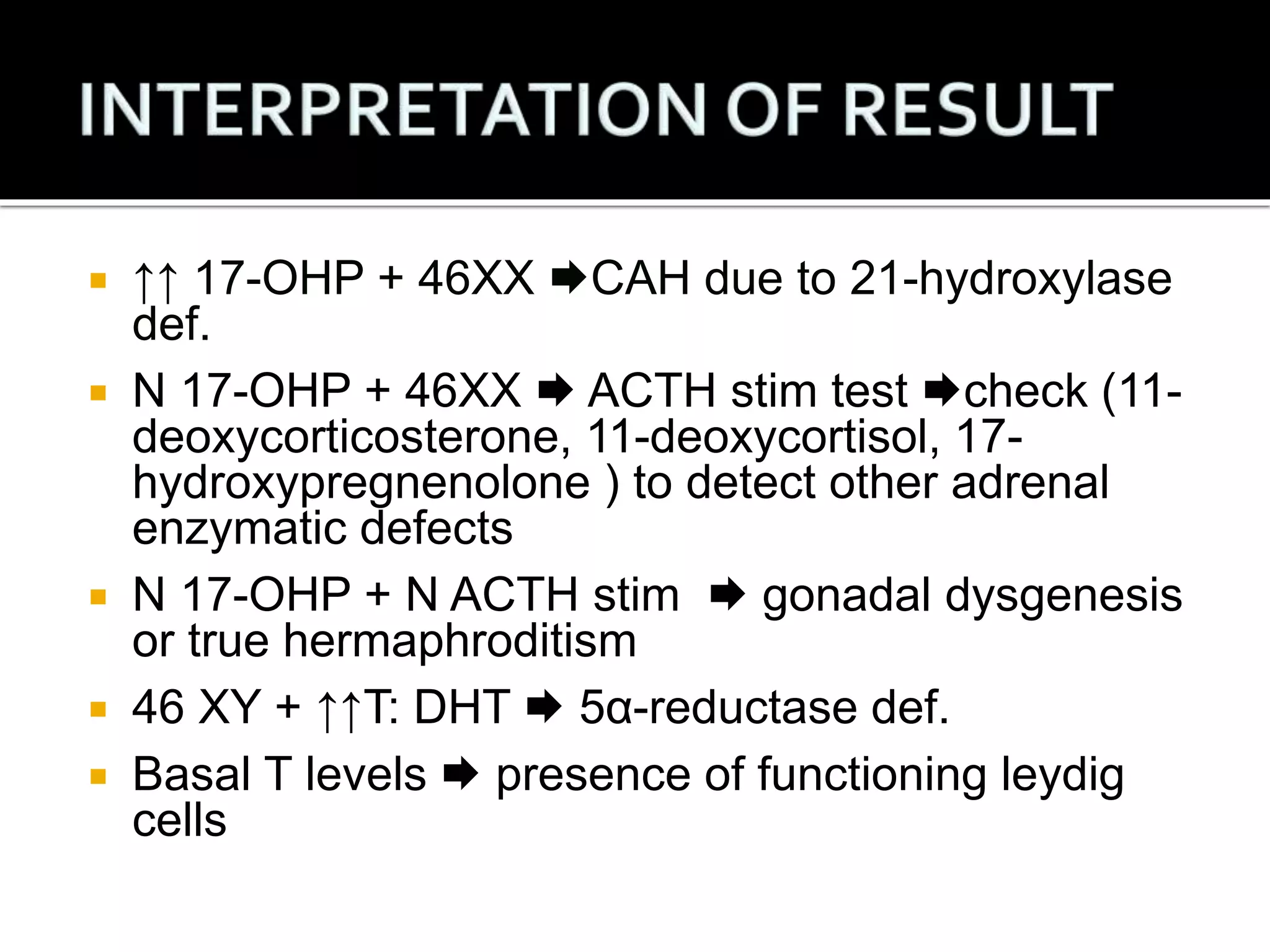
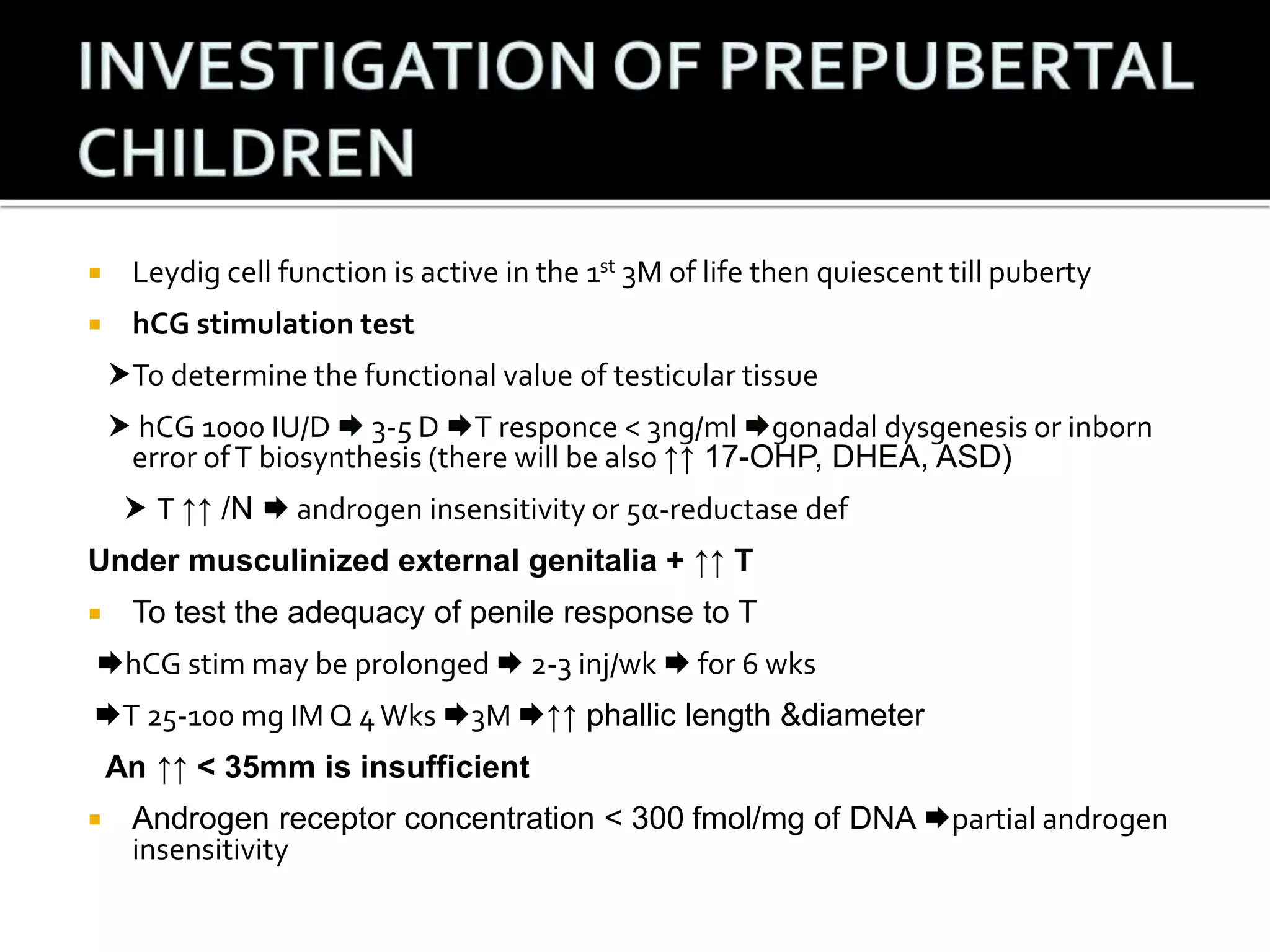
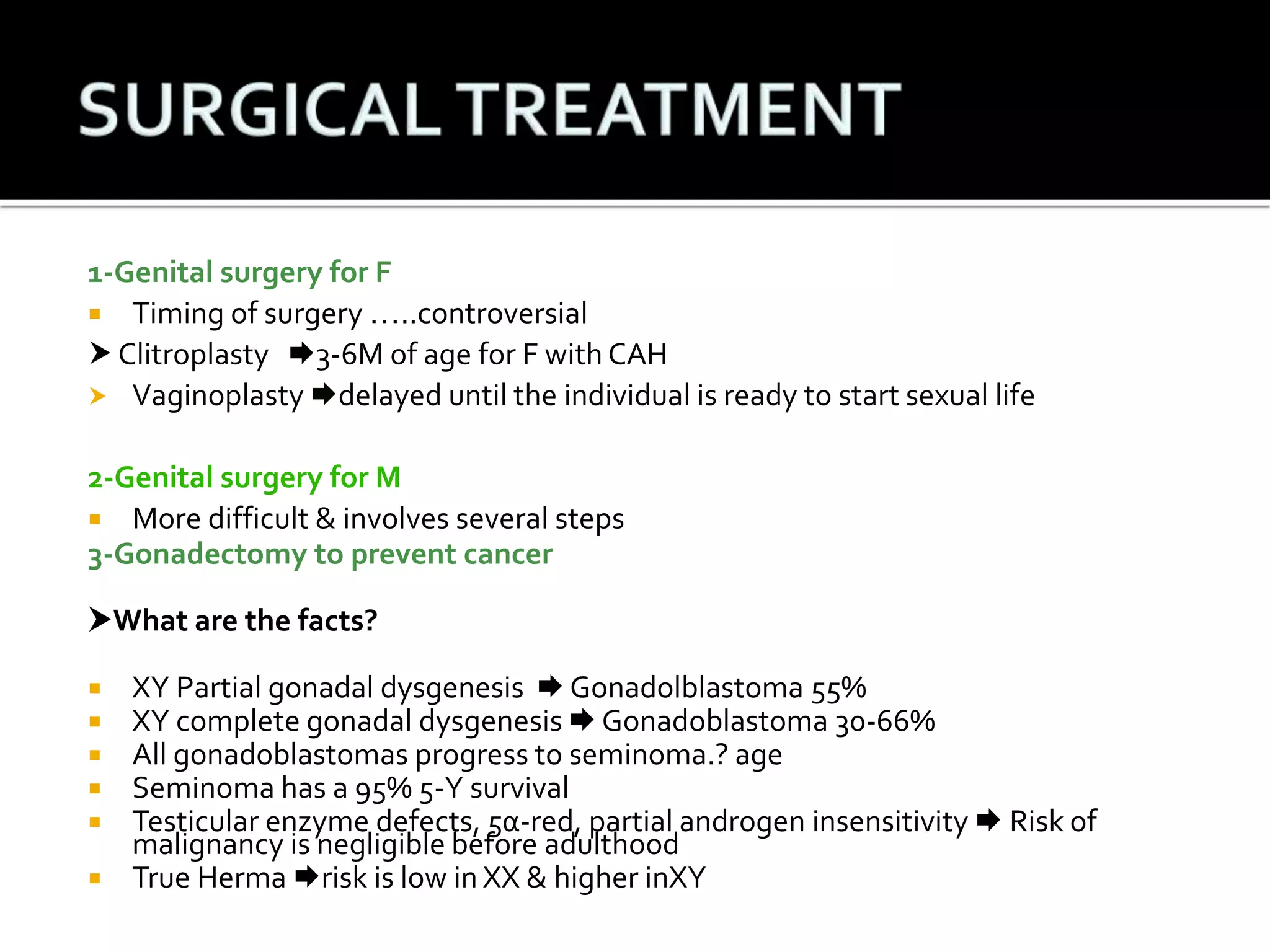
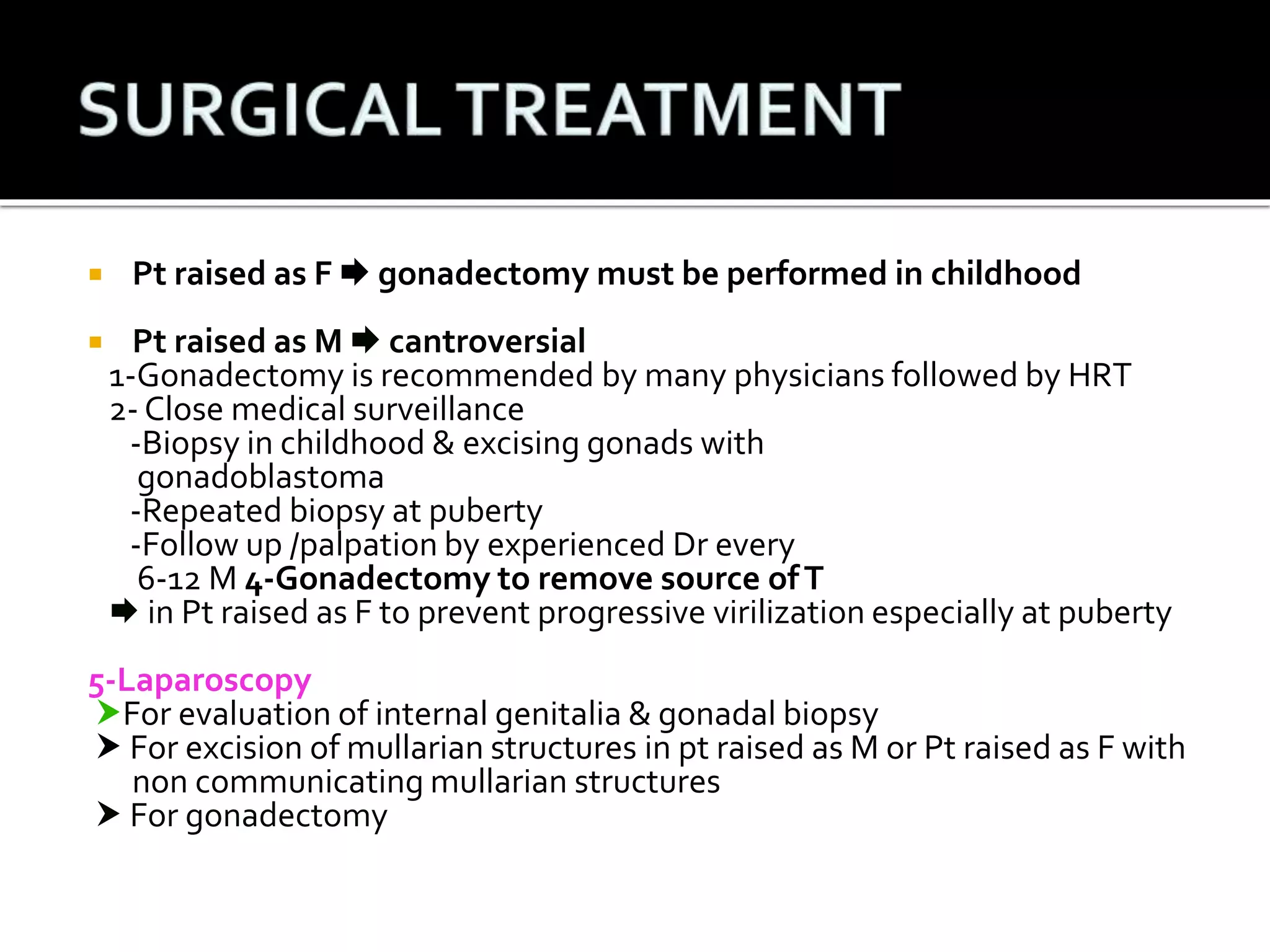
The document provides an overview of disorders of sex development (DSD) covering aspects of embryological development, key genetic factors, and hormonal influences in sexual differentiation. It discusses various DSD types linked to chromosomal anomalies and hormonal deficiencies, such as congenital adrenal hyperplasia, androgen insensitivity, and other genetic syndromes. Additionally, it includes clinical presentations, laboratory findings, and therapeutic interventions for affected individuals.