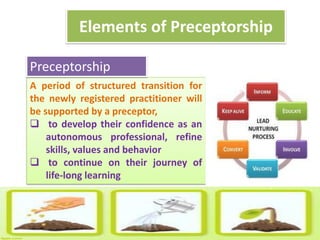
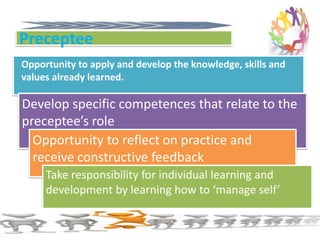
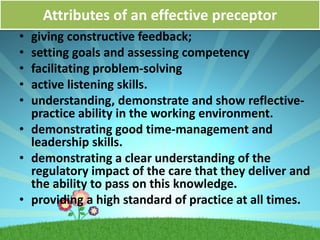
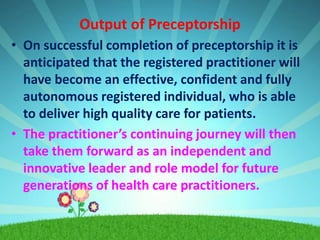
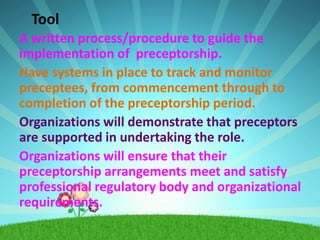
This document provides an overview and framework for preceptorship programs. It aims to support new staff through orientation and role transitions. Key elements include pairing a new staff member with a preceptor to facilitate learning, develop competencies, and provide feedback. Benefits include increased confidence, job satisfaction, and quality of care for patients. Effective preceptors act as role models, provide constructive feedback, and facilitate problem-solving skills. Upon completion, new staff should be confident and autonomous in delivering high quality care. The framework provides standards and tools to guide preceptorship implementation and monitoring.