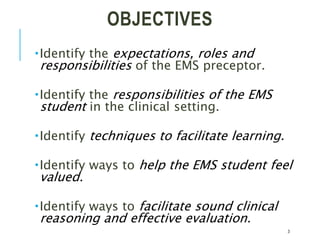
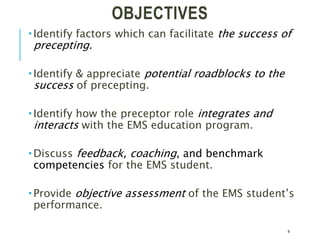
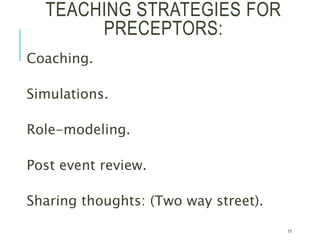
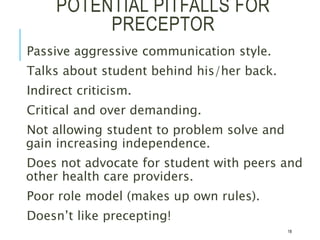
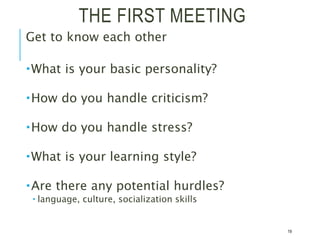
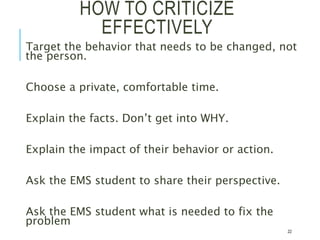
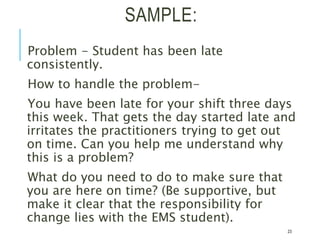
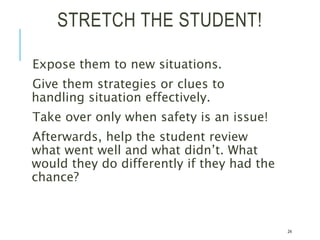
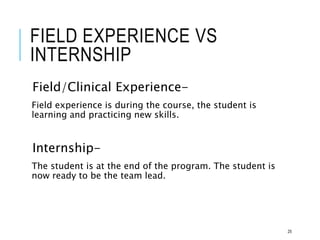
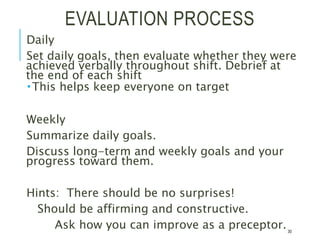
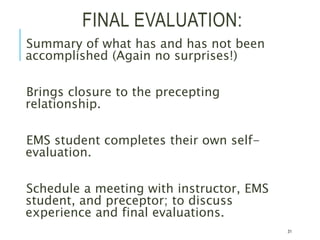
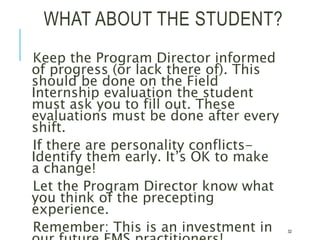
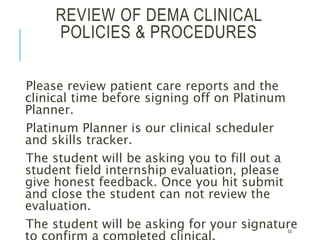
The document provides guidance for preceptors training to work with EMS students. It outlines the purpose of preceptorship as facilitating student learning and transition to practice. Preceptors should serve as role models, provide feedback and gradually increase student responsibilities. Students are expected to be responsible, ask questions and work hard to learn skills. The preceptor's role is to orient, teach, ensure safety, and evaluate students, providing frequent, specific feedback to support learning.