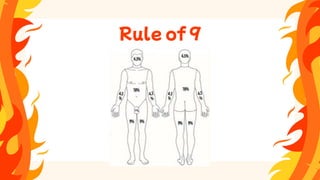
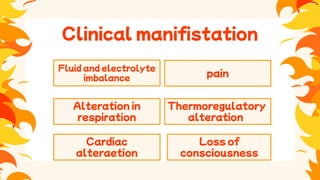
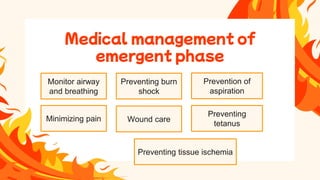
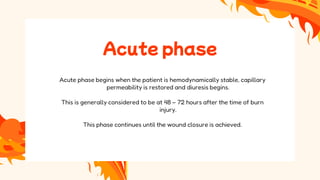
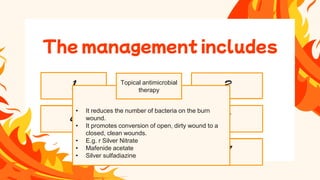
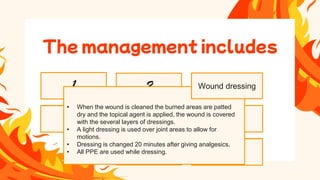
The document outlines the types, causes, and classifications of burns, including thermal, chemical, electrical, radiation, and inhalation injuries, as well as their pre-hospital care and medical management. It details the clinical manifestations associated with burns, such as fluid and electrolyte imbalances, cardiac alterations, and pain, while describing the phases of burn treatment from the emergent phase to rehabilitation. Comprehensive management strategies, including fluid resuscitation, pain control, infection prevention, and the use of topical antimicrobial therapy, are emphasized for effective treatment of burn victims.