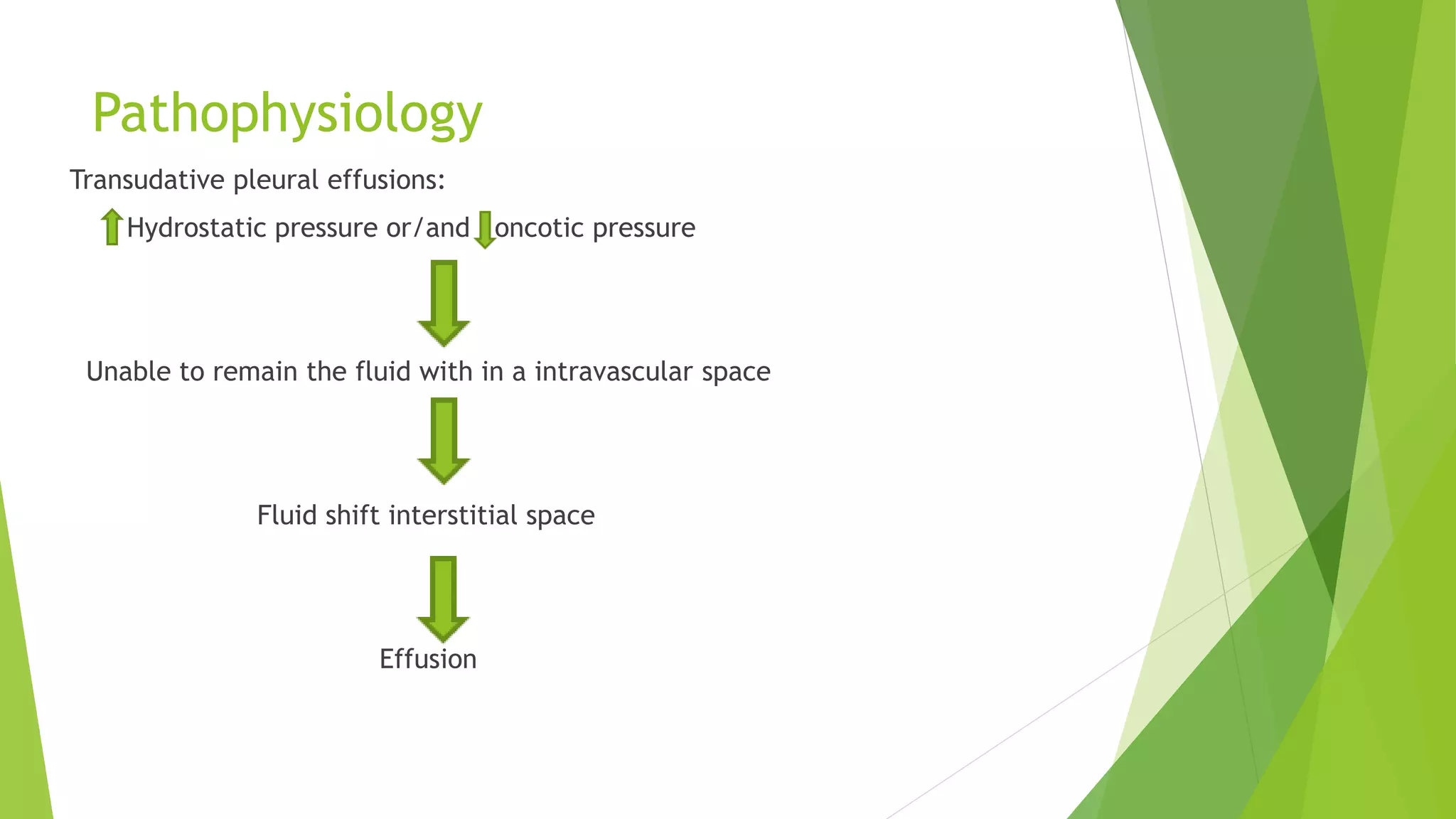
This document discusses pleural effusion, which is an abnormal accumulation of fluid in the pleural space between the lungs and chest wall. Pleural effusions are classified as transudative or exudative based on the fluid characteristics. Transudative effusions are low protein fluids caused by conditions that increase hydrostatic pressure or decrease oncotic pressure like heart failure or liver disease. Exudative effusions are high protein fluids caused by inflammation from conditions such as pneumonia, tuberculosis, or malignancy. Diagnosis involves chest x-rays, ultrasound, or thoracentesis to analyze the fluid. Treatment focuses on identifying and treating the underlying cause while relieving symptoms through thoracentesis if needed.