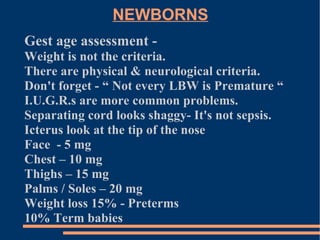
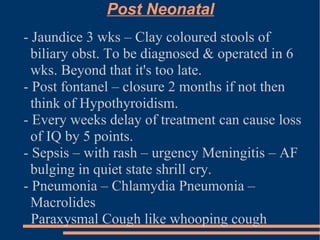
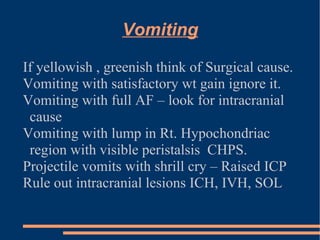
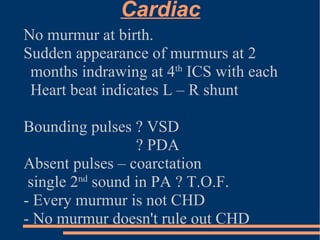
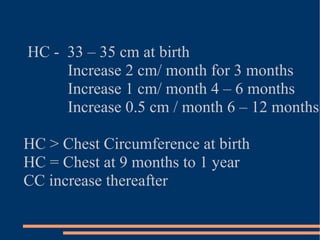
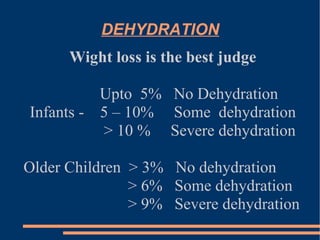
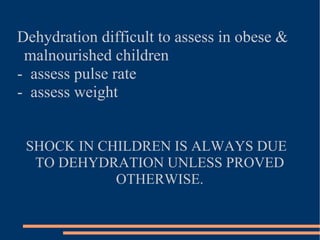
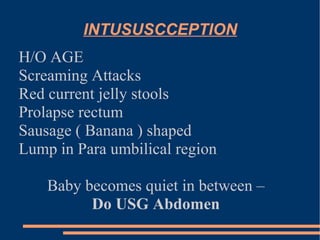
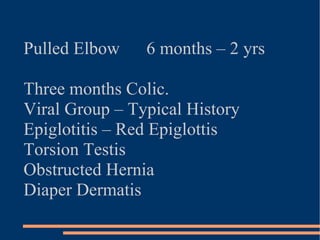
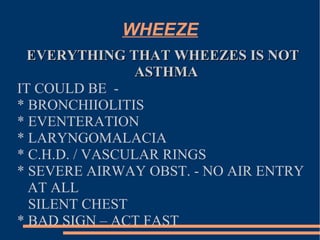
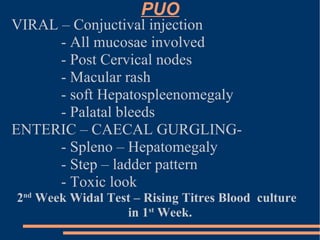
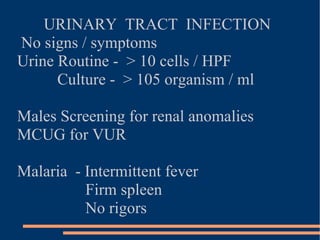
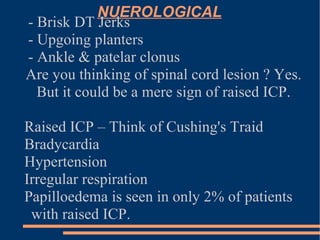
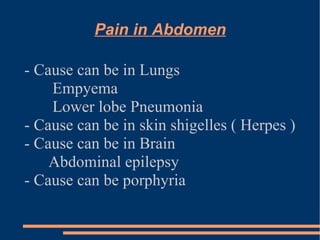
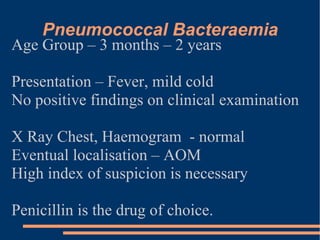
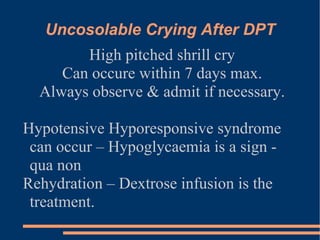
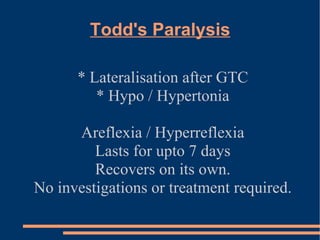
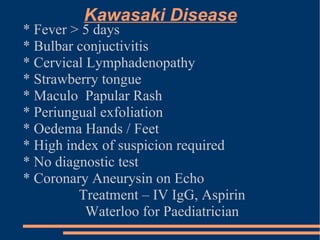
This document provides guidance on common pitfalls in pediatric practice. It discusses accurate assessment of newborns, including gestational age and causes of jaundice. Common issues are outlined for post-neonatal periods up to age 3, including causes of vomiting, cardiac murmurs, growth monitoring, and dehydration assessment. Guidance is provided on intussusception, pulmonary conditions, urinary tract infections, and neurological signs. Specific conditions like Kawasaki disease are also summarized. The document emphasizes considering diverse potential causes and having a high index of suspicion to correctly diagnose common pediatric problems.