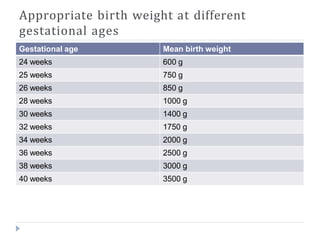
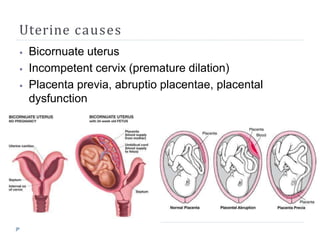
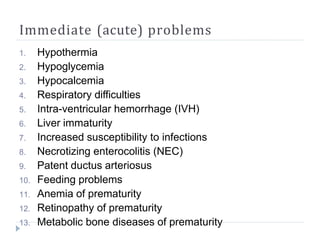
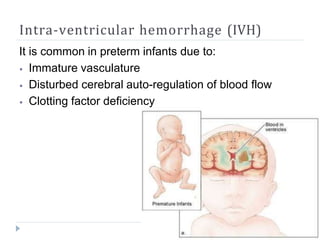
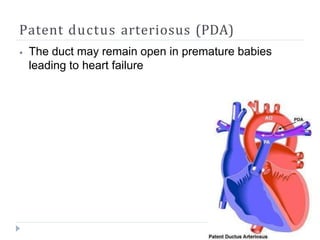
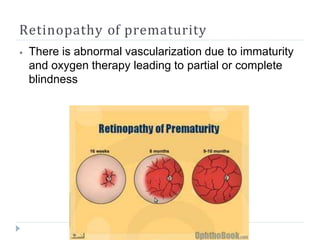
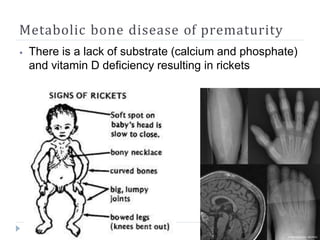
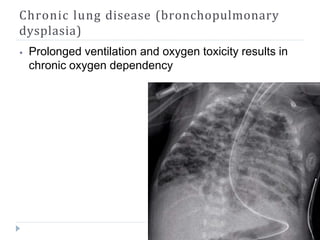
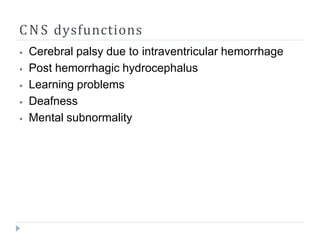
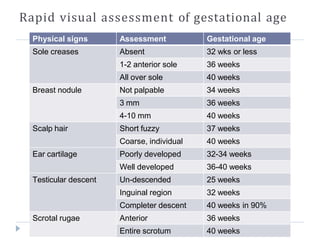
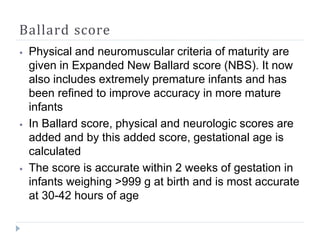
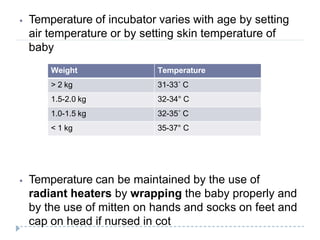
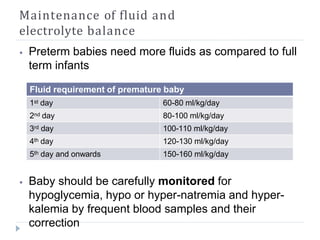
This document discusses prematurity and its complications. It defines prematurity as a live birth before 37 weeks gestation. The incidence in Pakistan is estimated at 11-13%. Immediate complications of prematurity include hypothermia, hypoglycemia, respiratory issues, infections, and bleeding in the brain. Long term complications can include lung and brain issues. Management involves careful delivery, maintaining temperature and fluids, limiting oxygen exposure, appropriate feeding, and preventing infections. Outcomes are improved with anticipating and preventing complications of prematurity.