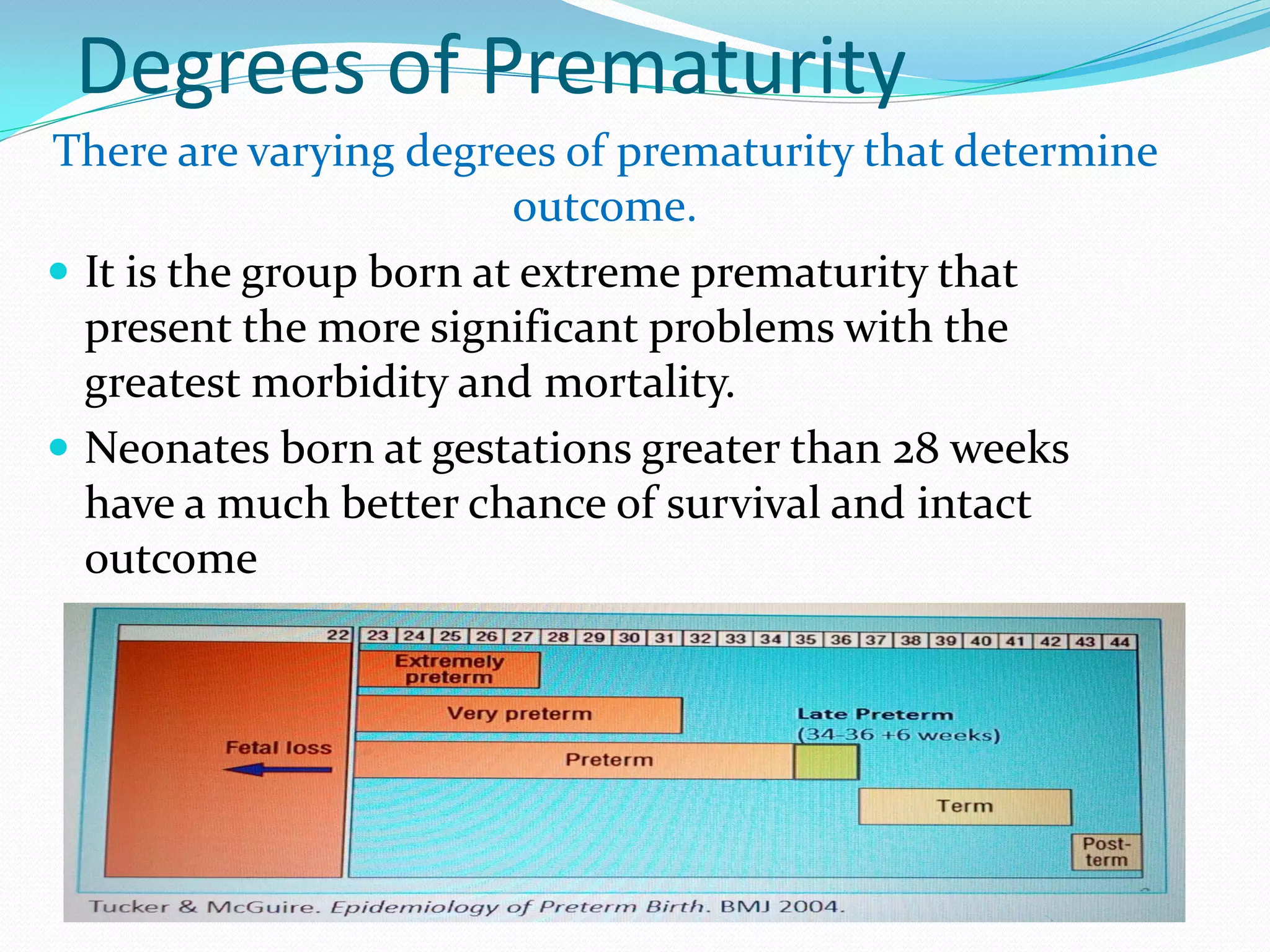
The document discusses preterm birth and summarizes key information. It defines a preterm baby as one delivered before 37 weeks of gestation. Worldwide, preterm birth complicates 5-18% of births, with rates of 5-9% in Europe and 12-13% in the USA. Prematurity is associated with short and long term complications affecting multiple organ systems. Prevention strategies aim to reduce preterm birth through screening and treating at-risk women. Treatment includes steroids, antibiotics, tocolysis and neonatal care to improve outcomes.