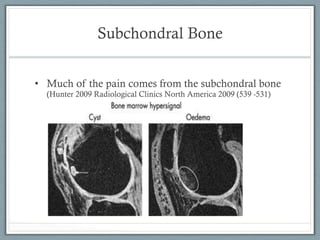
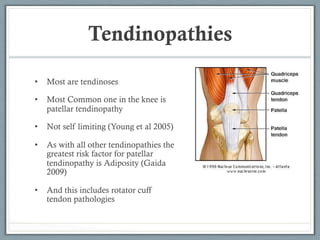
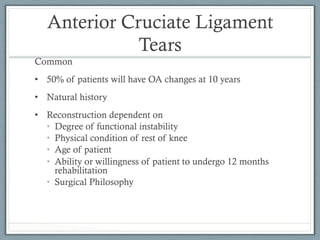
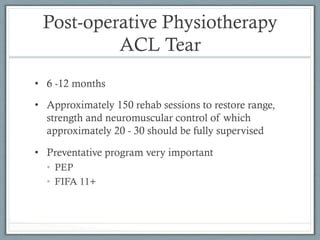
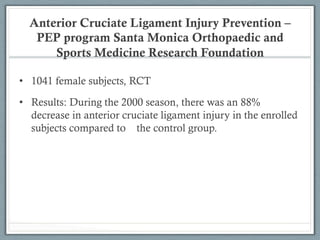
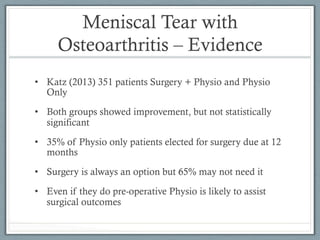
The document outlines the physiotherapy management of common knee problems, emphasizing contemporary treatment models for conditions like osteoarthritis, tendinopathies, and ligament injuries. It discusses necessary rehabilitation phases, exercise recommendations, and various management strategies aimed at restoring function, preventing re-injury, and optimizing patient outcomes. Key recommendations include self-management, weight loss for patients with osteoarthritis, and the importance of pre-operative and post-operative physiotherapy for conditions like ACL tears.