The document discusses physiotherapy for reconstructive hand surgery. It covers:
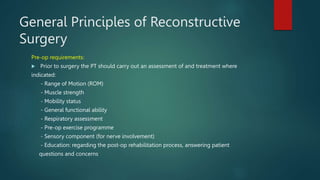
1. Pre-operative physiotherapy assessment and treatment including range of motion, strength, mobility and respiratory assessment.
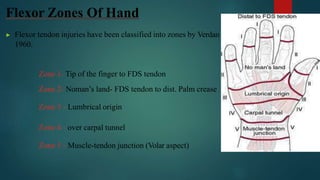
2. Common hand surgeries like tendon repairs, amputations, and arthritis conditions. Flexor tendon injuries are classified into zones.
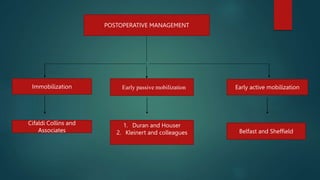
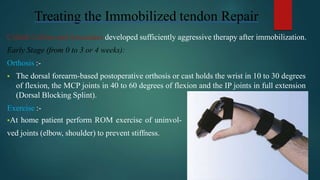
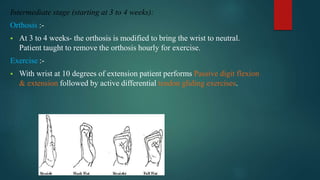
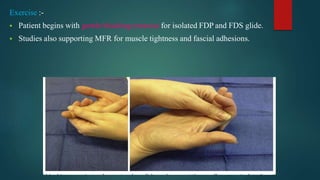
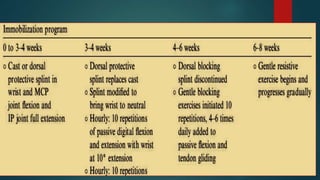
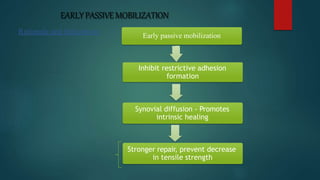
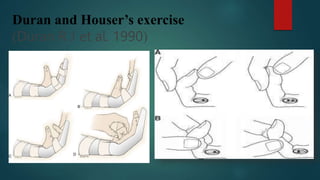
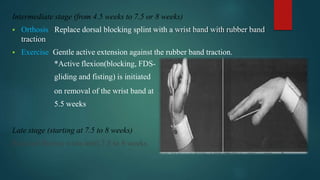
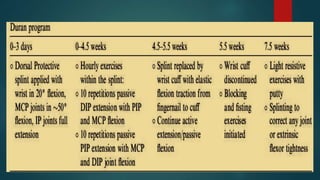
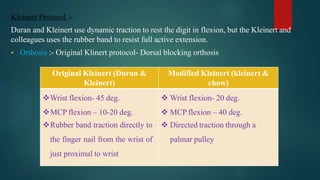
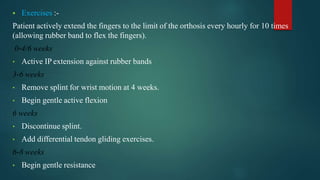
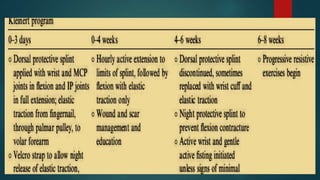
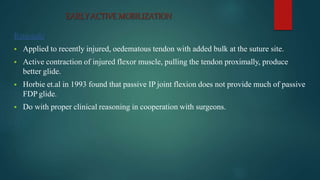
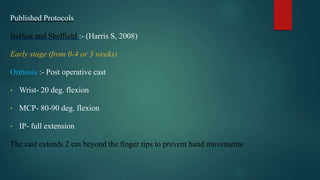
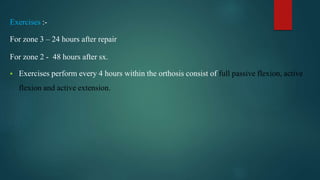
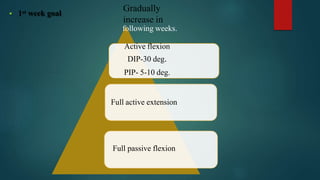
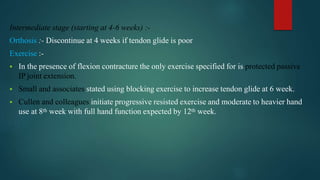
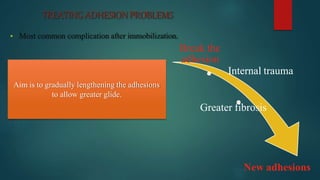
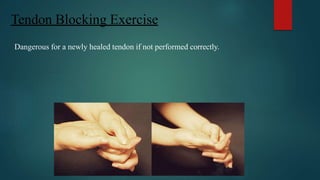
3. Post-operative rehabilitation protocols including immobilization, early passive motion, and early active motion. Exercises and progression of motion and strength over time are described for each protocol.