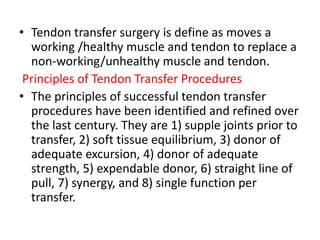
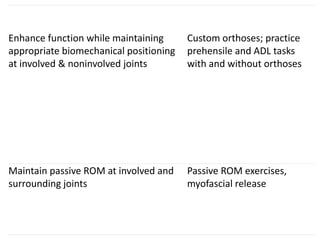
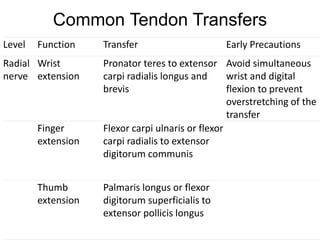
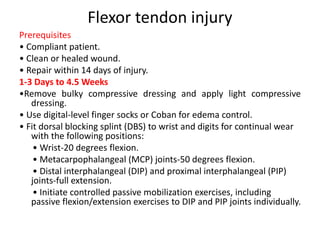
The document discusses post-operative management of tendon transfers and flexor/extensor tendon injuries. It outlines 3 phases of postoperative treatment: 1) immobilization, 2) activation of the transfer, and 3) strengthening/return to function. Specific protocols are provided for each phase including exercises, splinting, and precautions. Common tendon transfers are also reviewed for different nerve injuries along with prerequisites and rehabilitation guidelines.