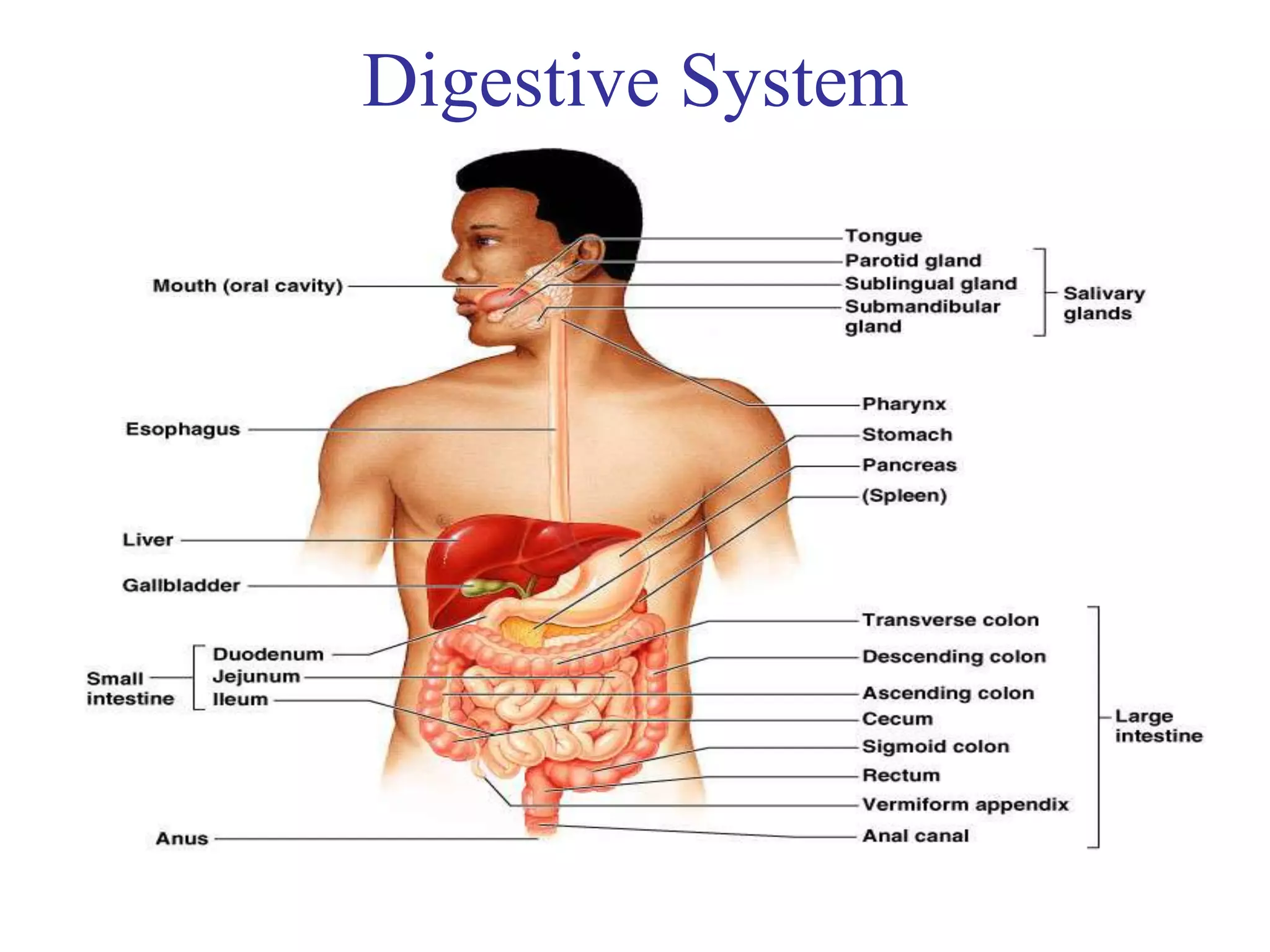
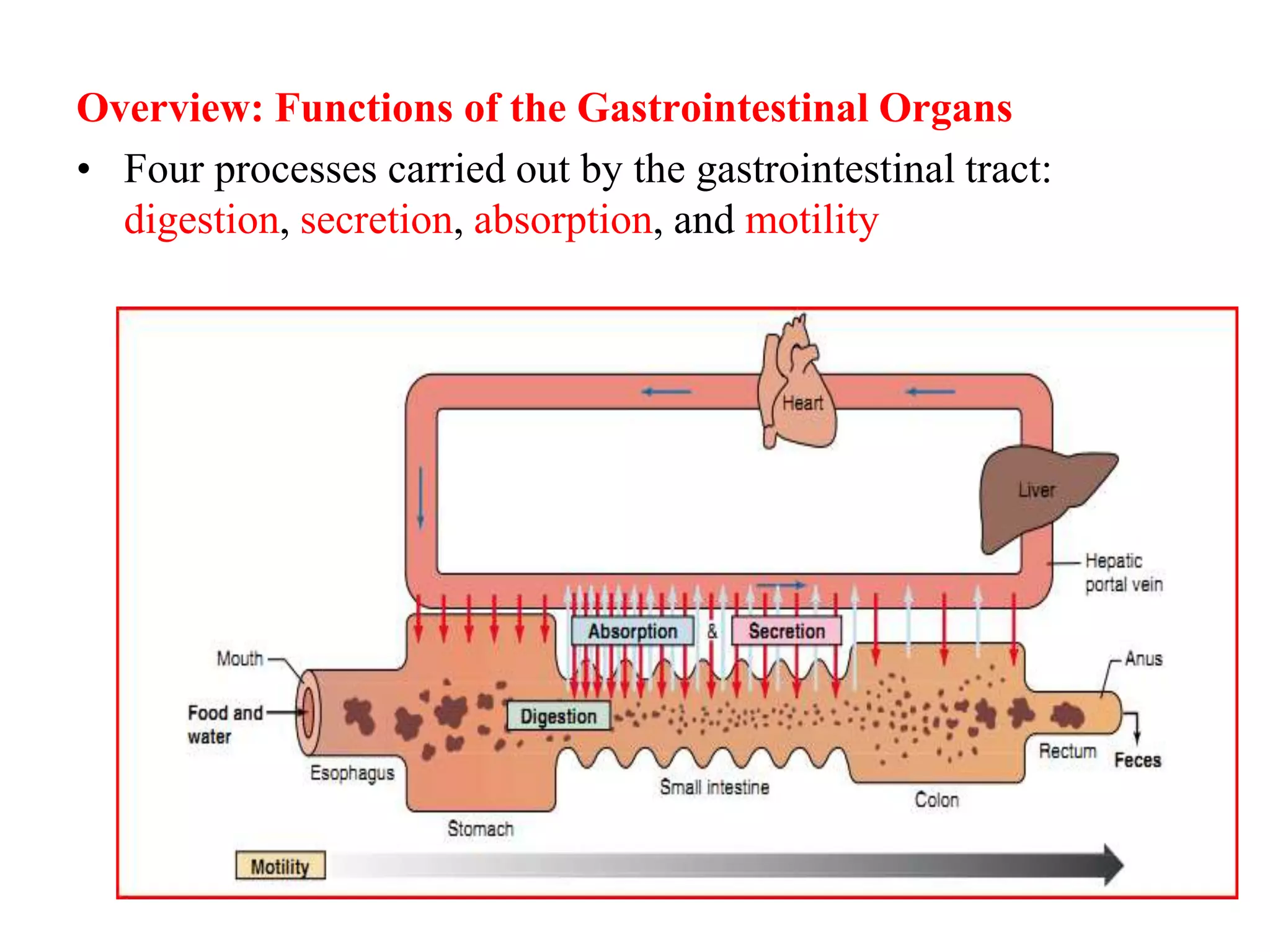
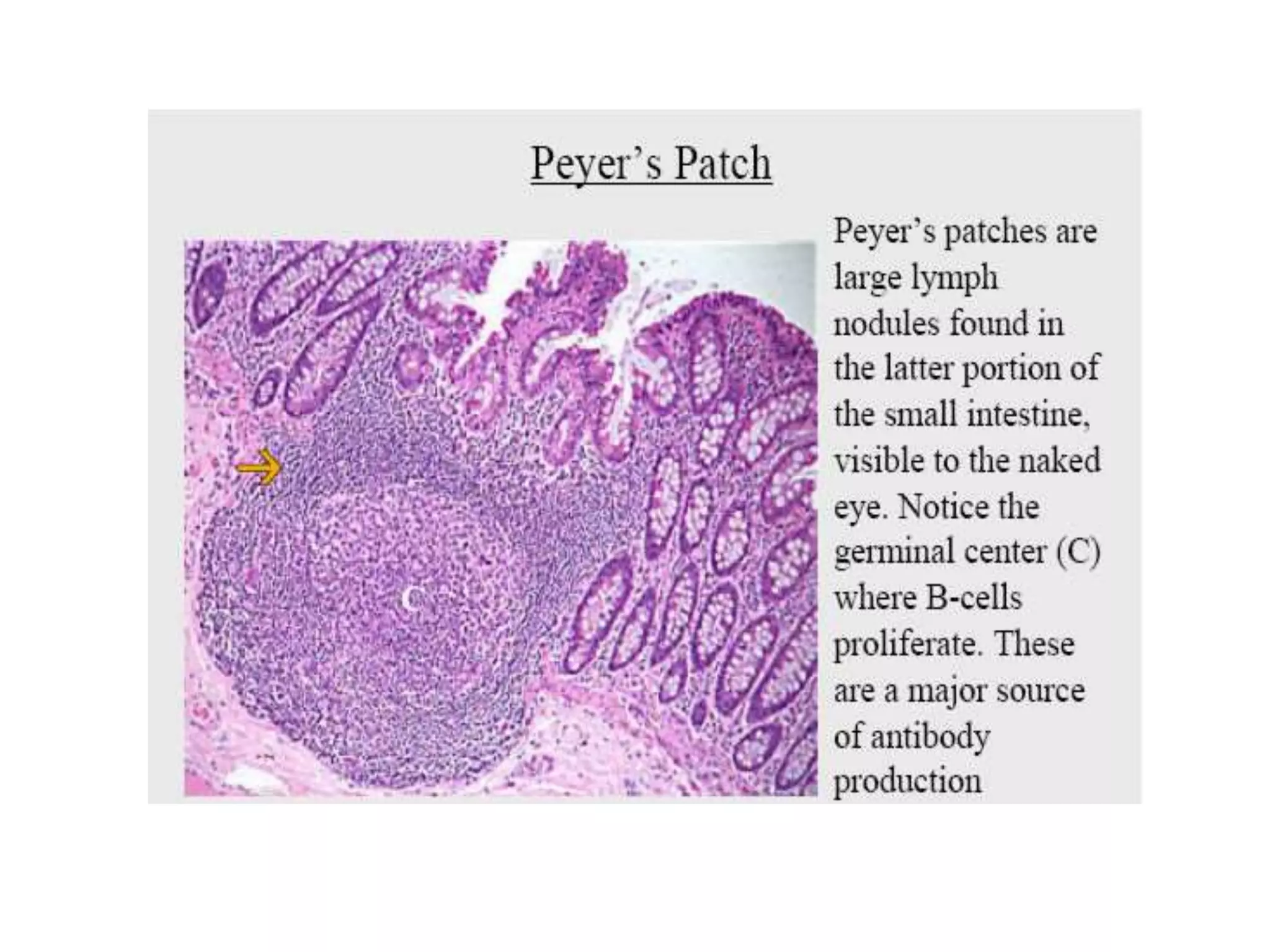
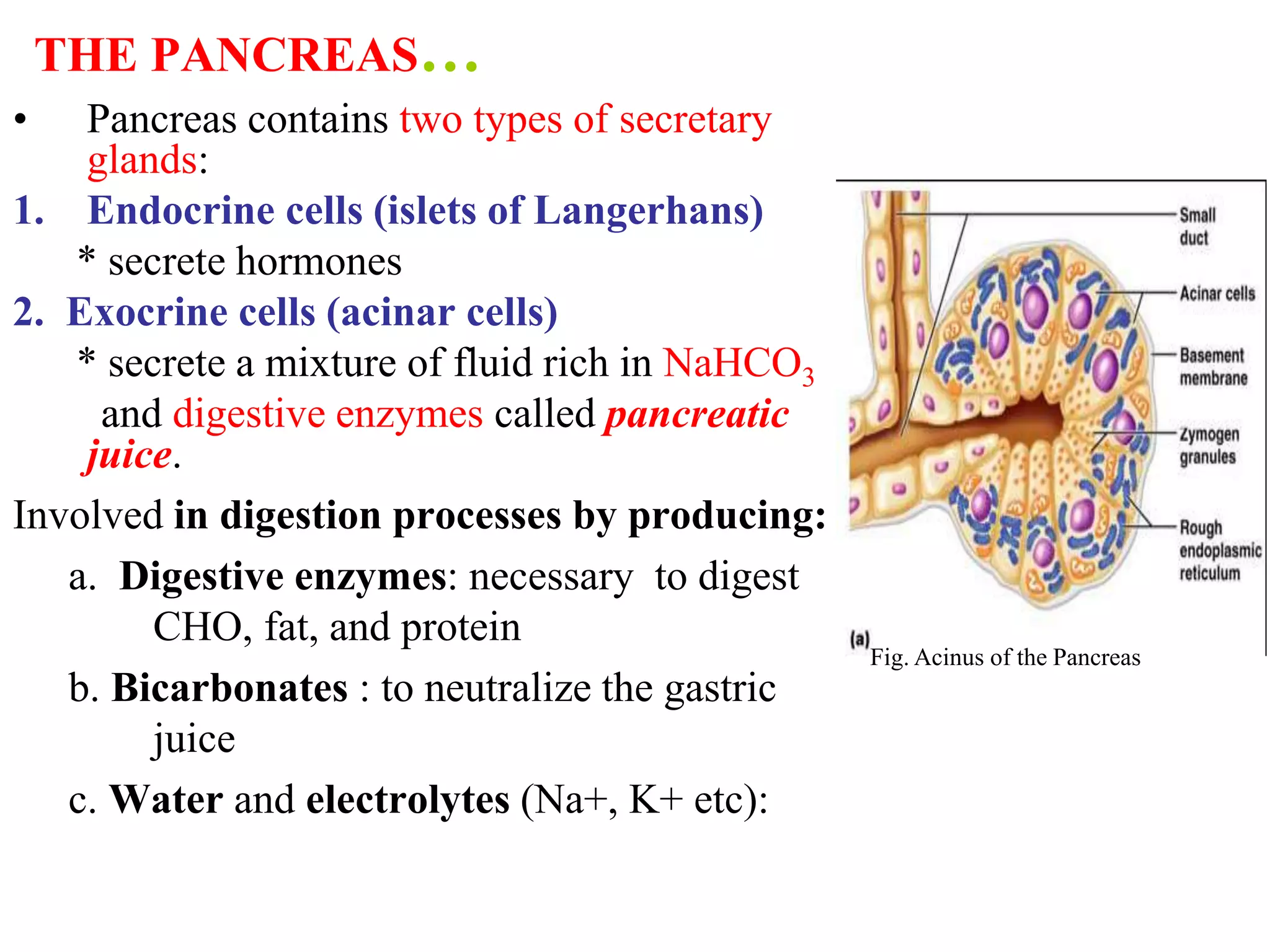
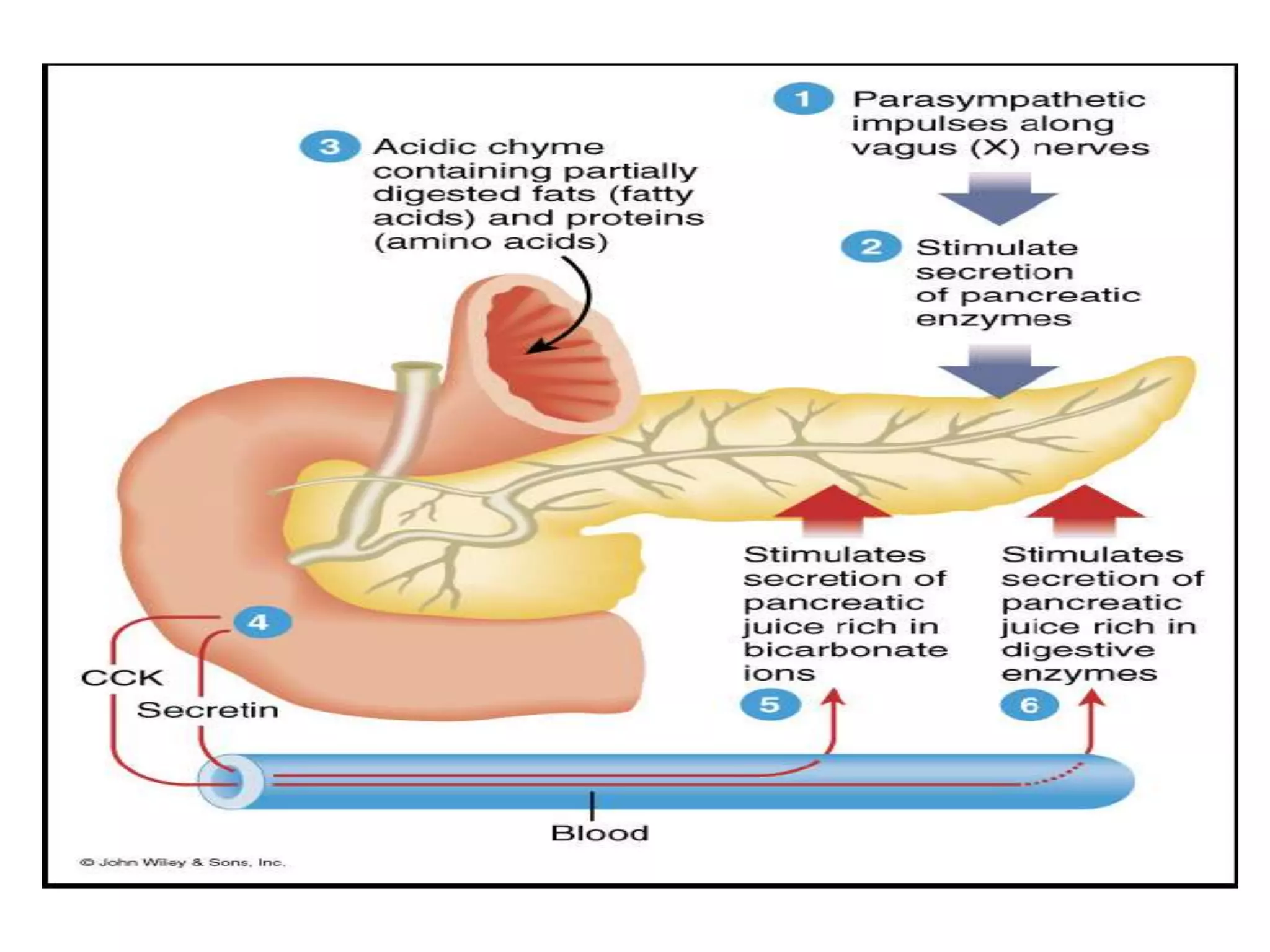
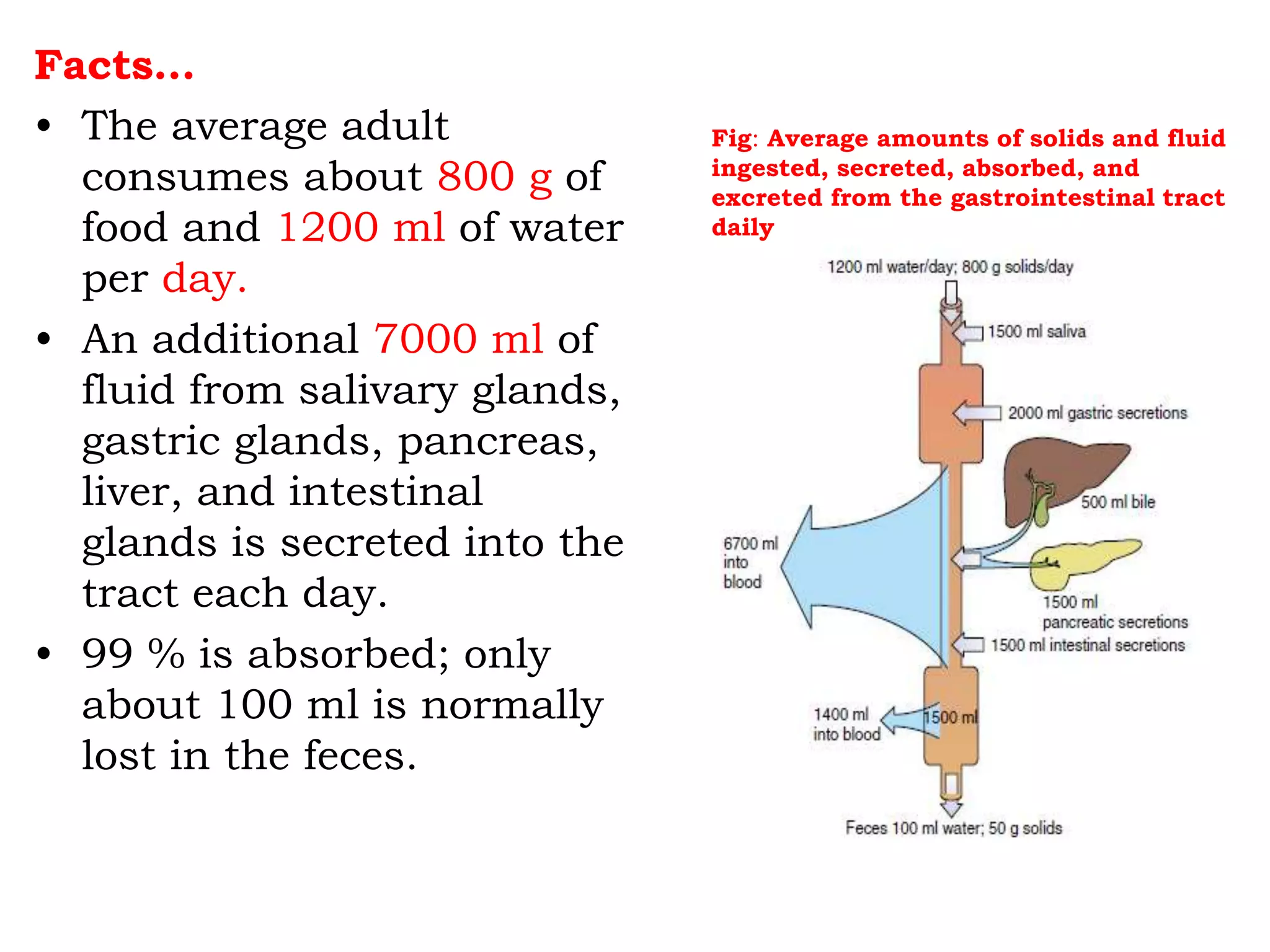
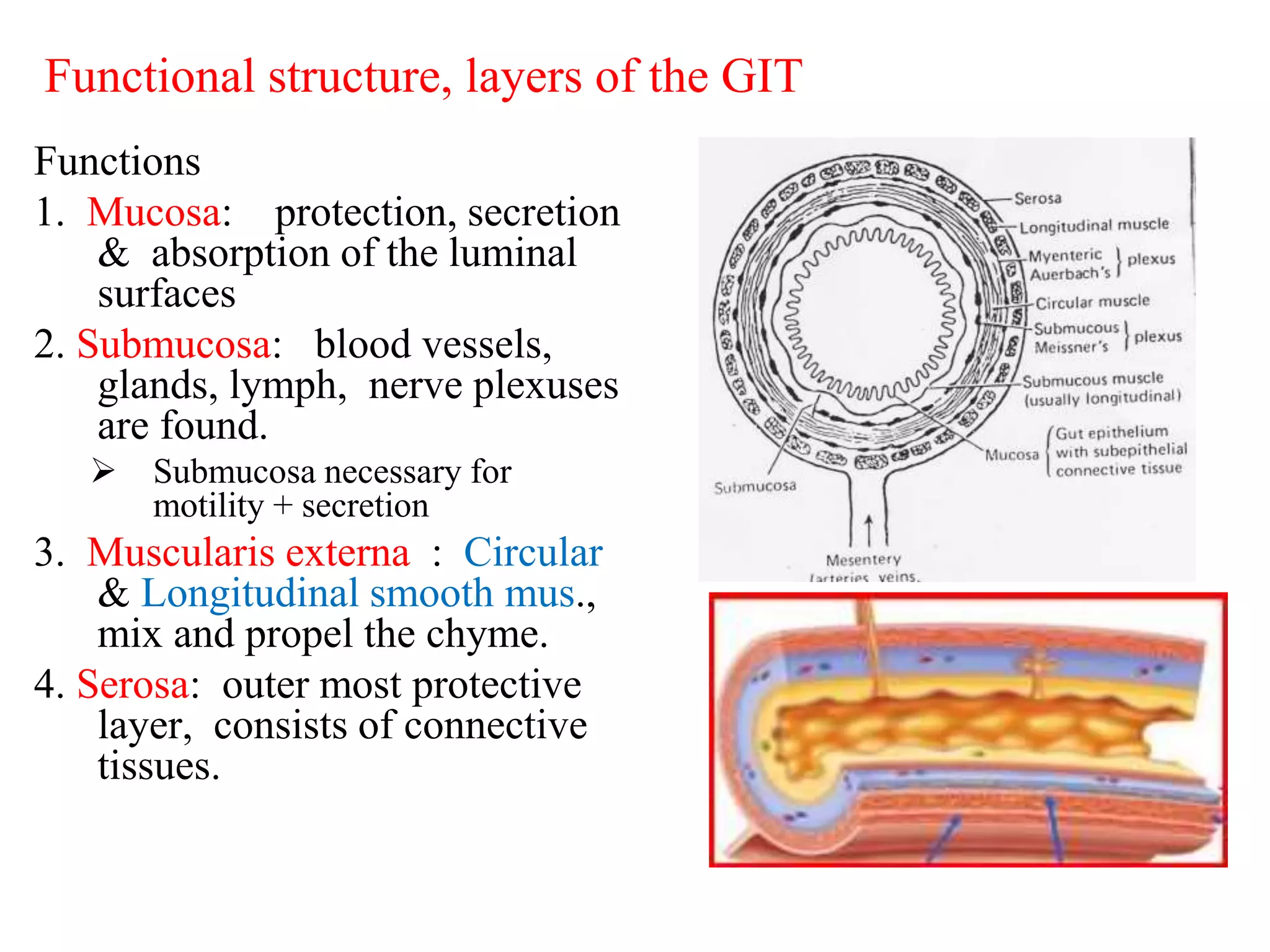
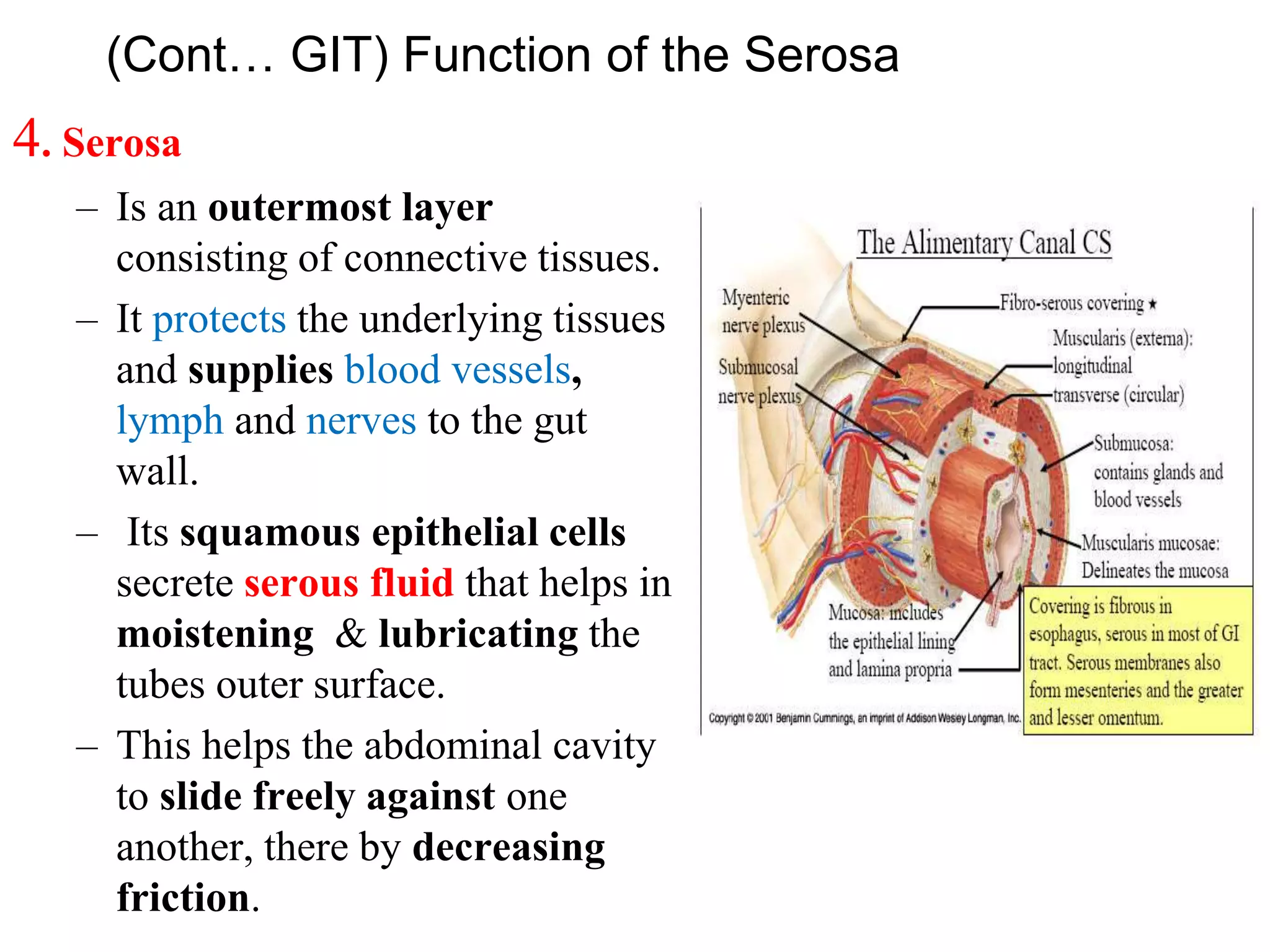
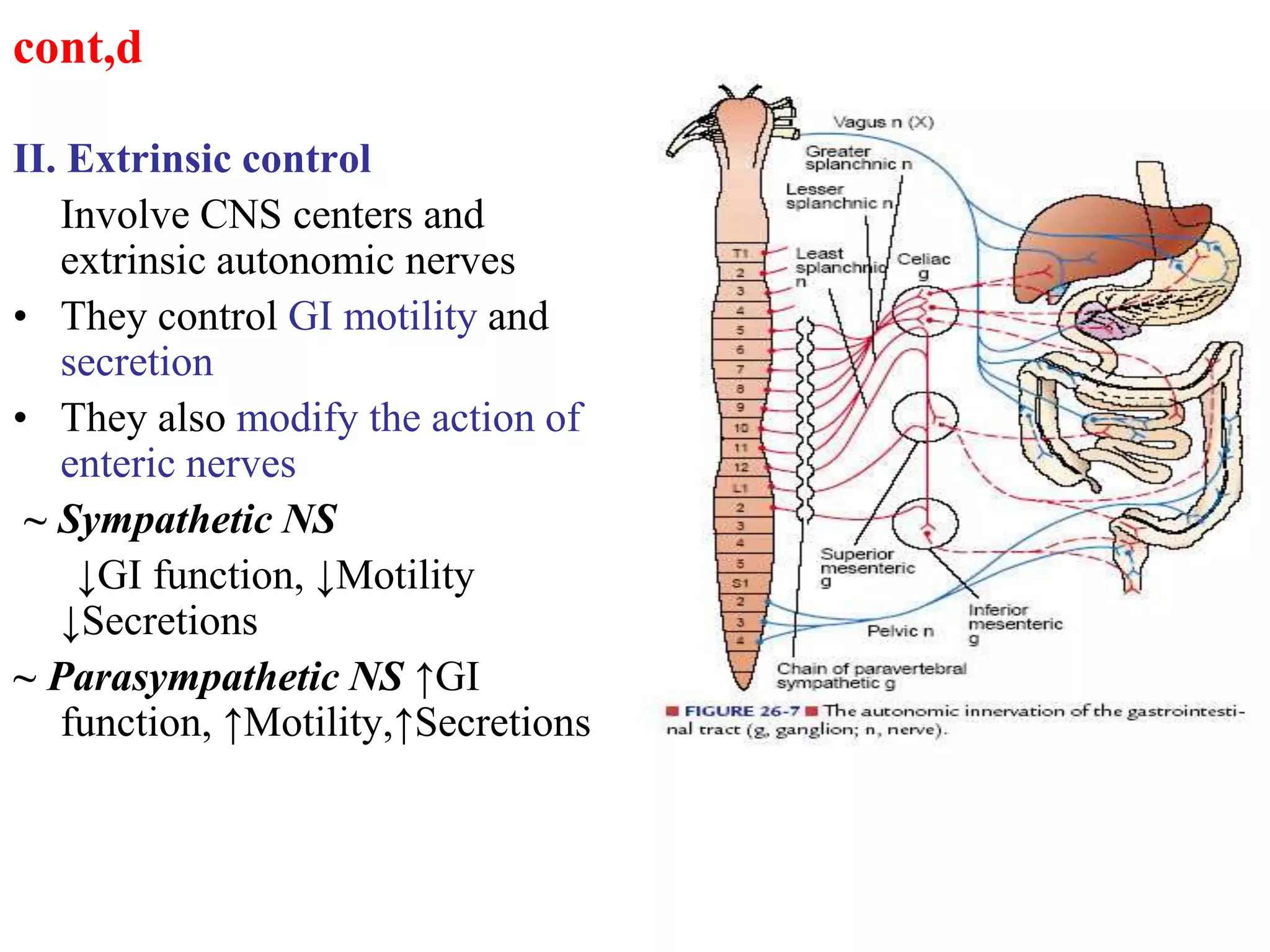
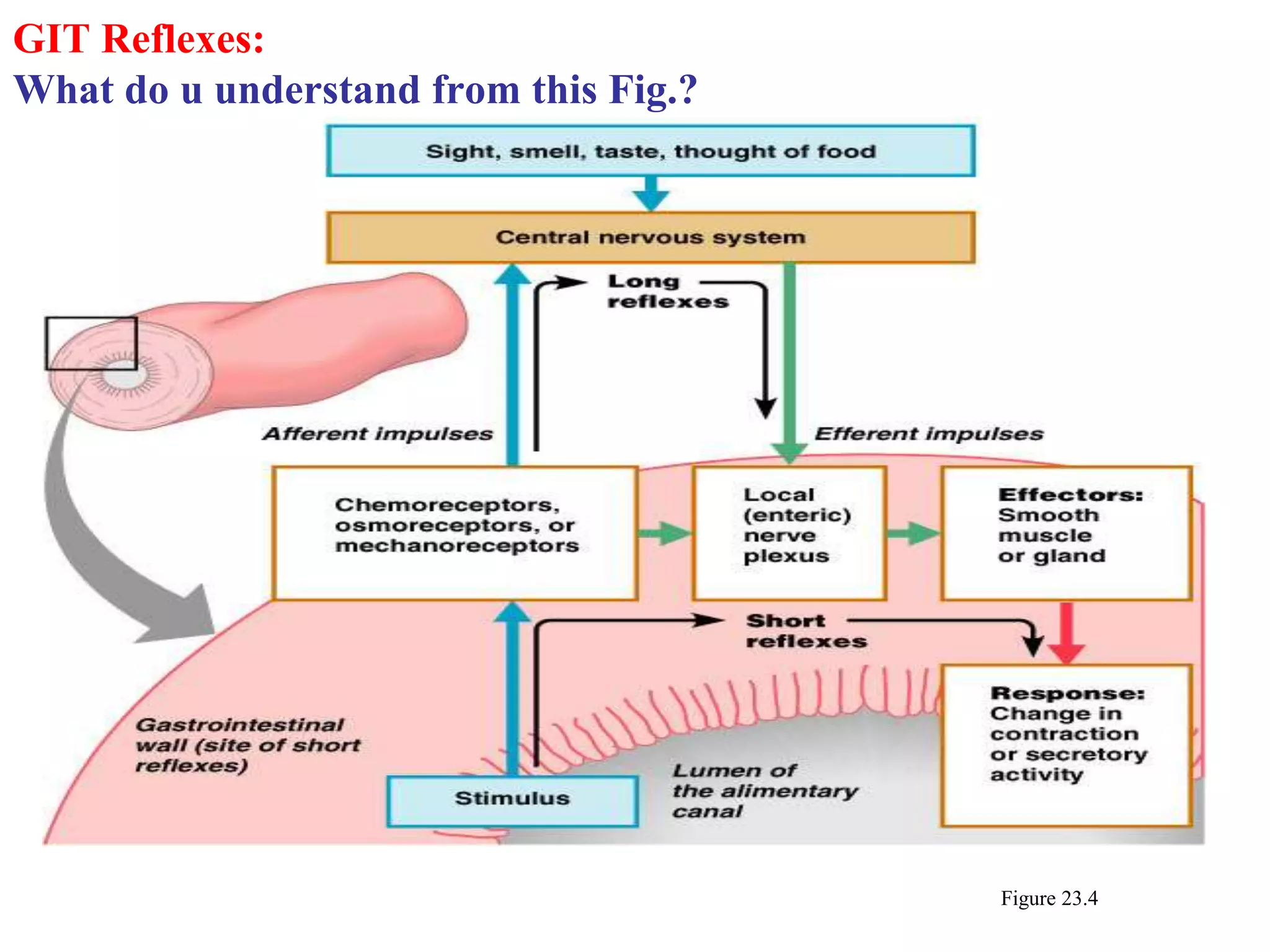
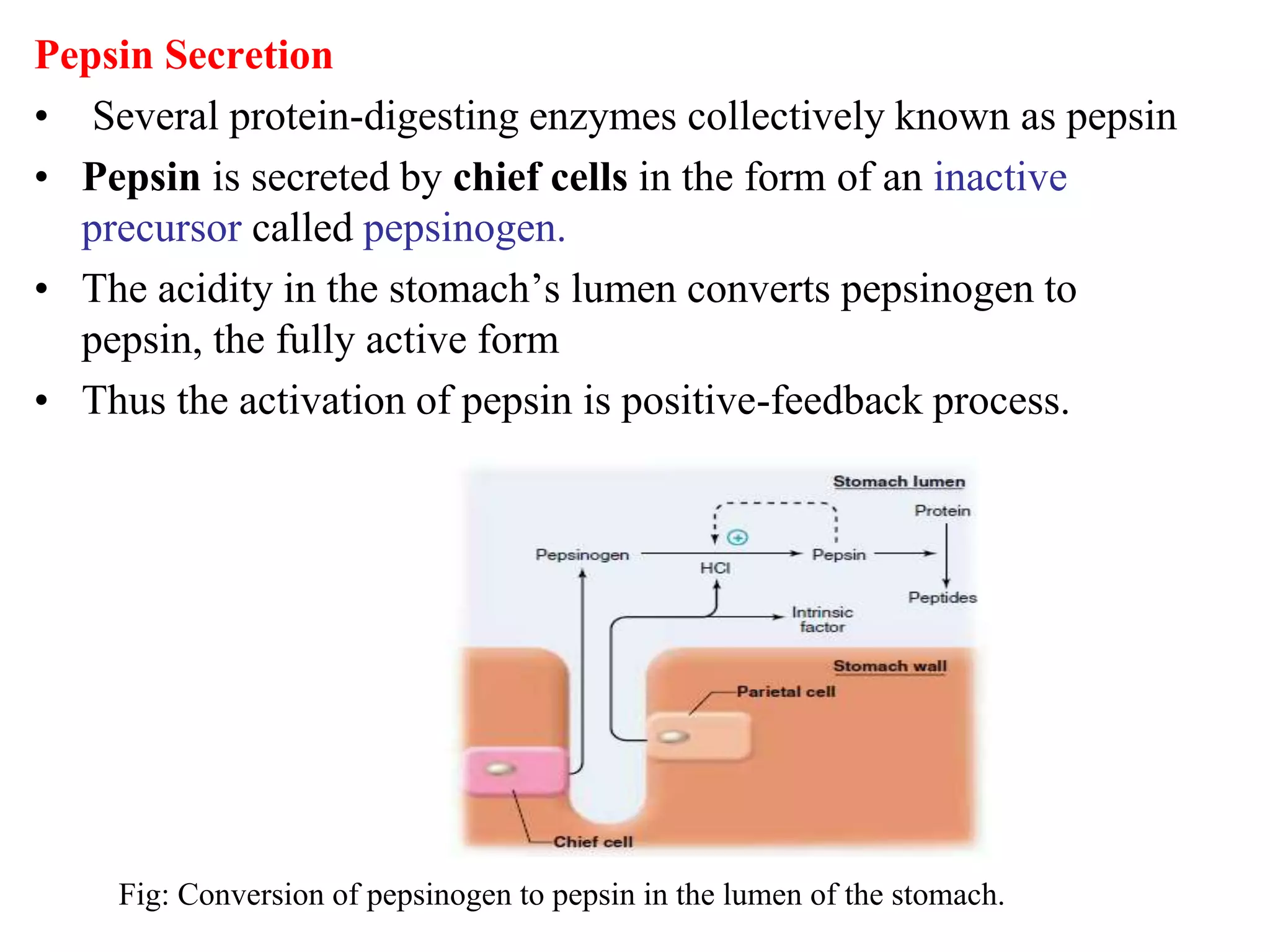
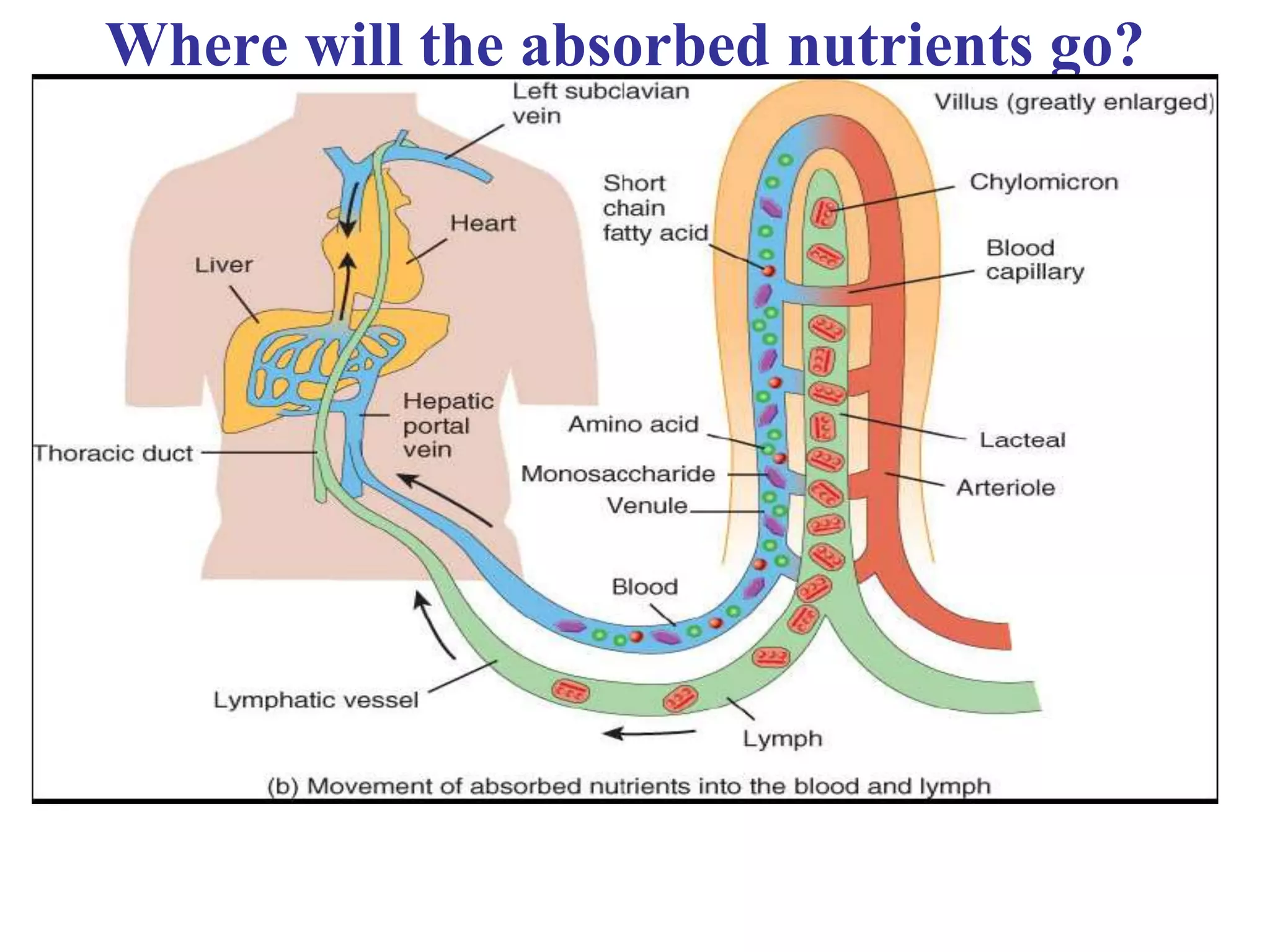
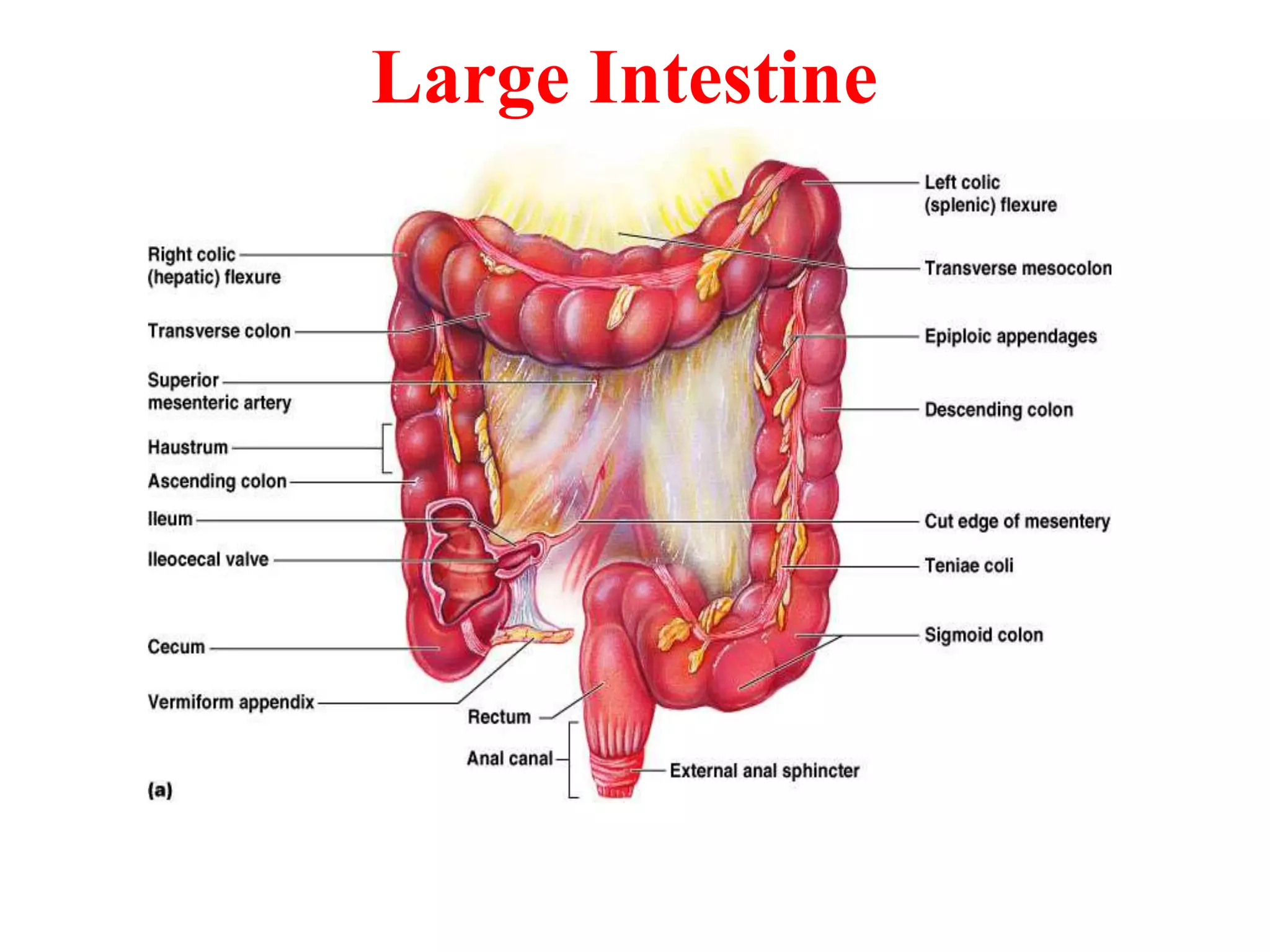
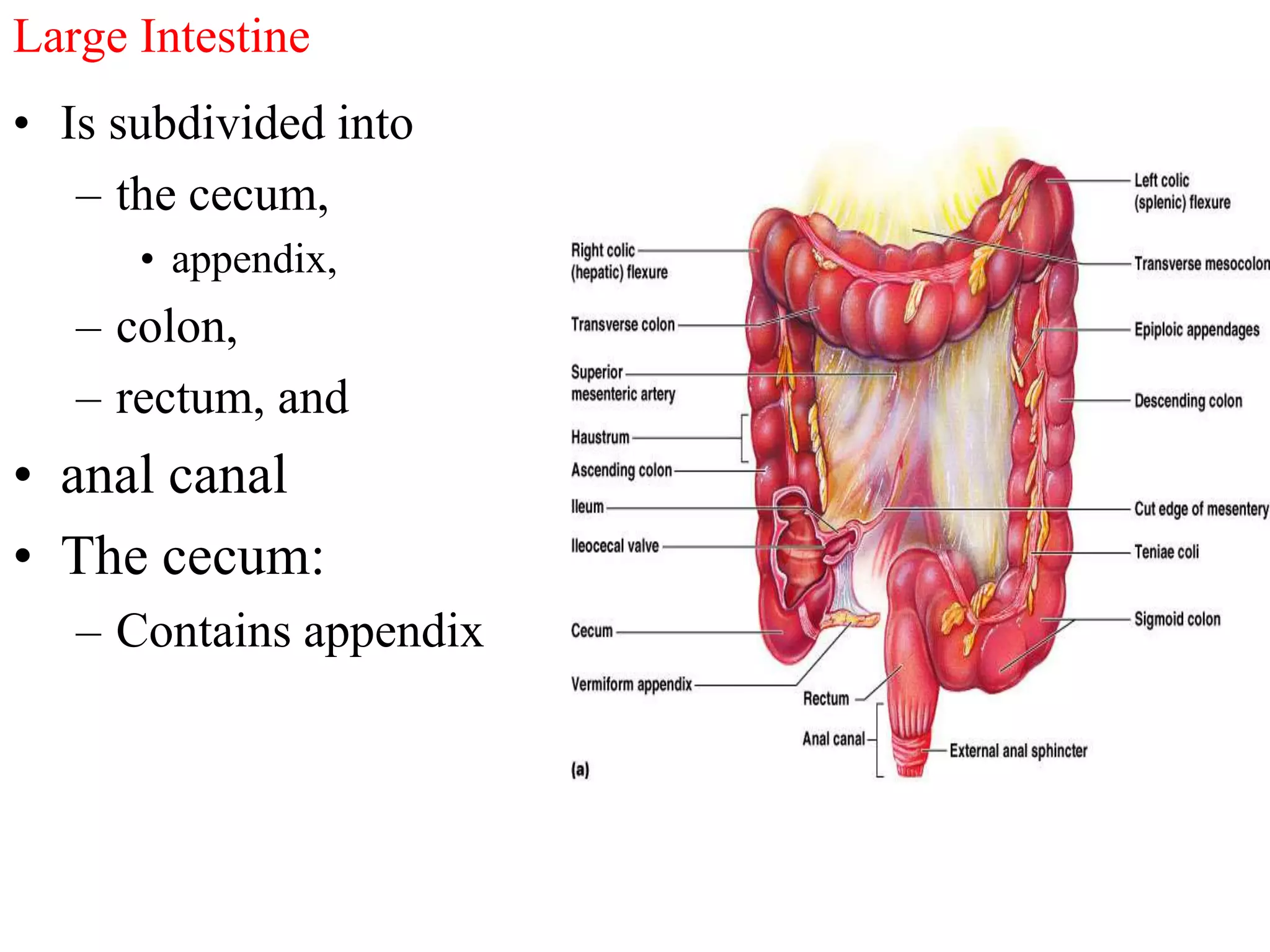
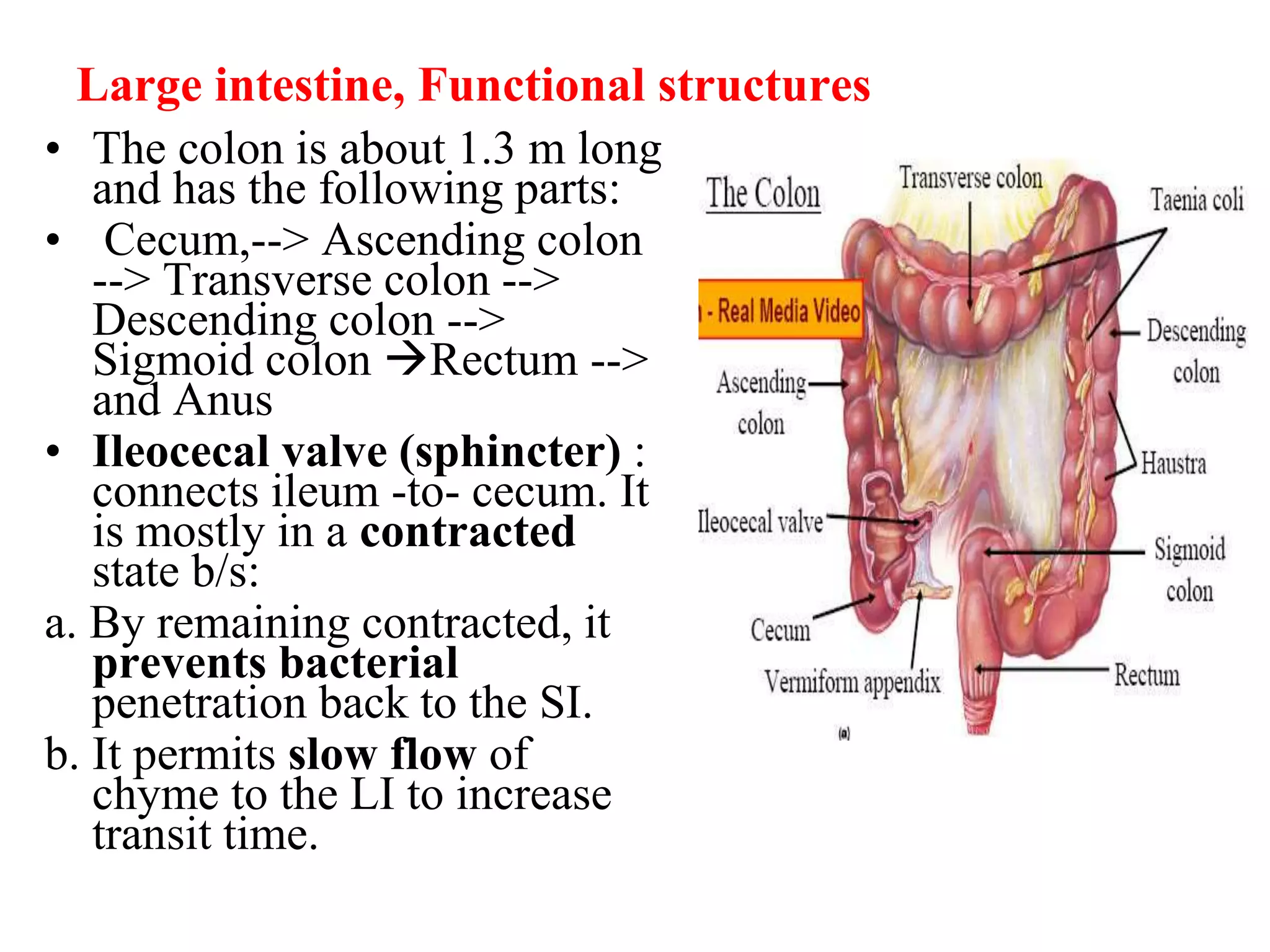
The document provides an overview of the physiology of the digestive system. It discusses the basic functions of the digestive system which include ingestion, digestion, absorption, and defecation. It describes the organs that make up the gastrointestinal tract (GIT) and their roles, including the mouth, esophagus, stomach, small intestine, large intestine, liver, gallbladder and pancreas. It also discusses the layers of the GIT wall, regulation of digestive functions by nerves and hormones, and the roles of saliva, stomach secretions, bile, and pancreatic juices in digestion.