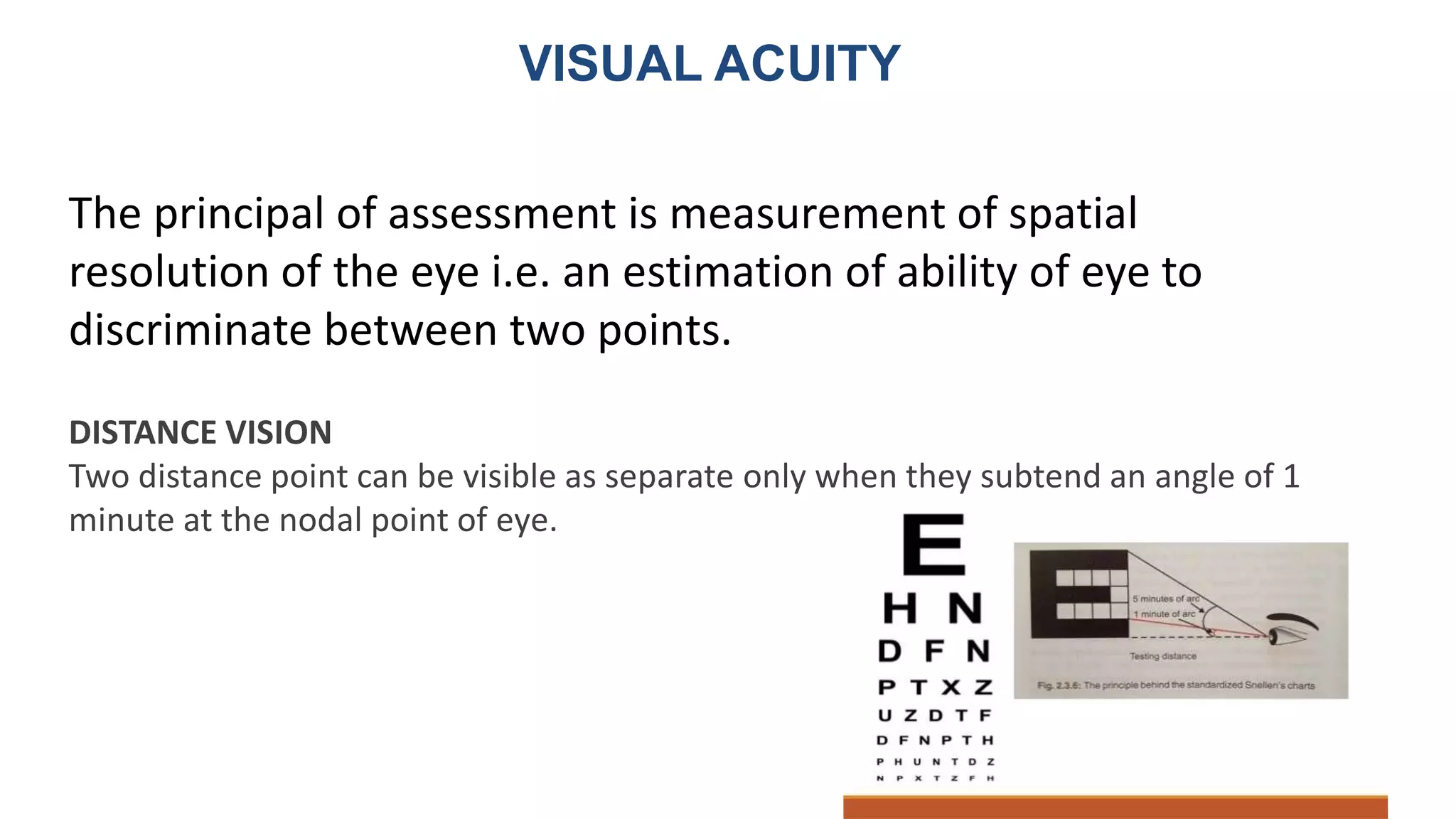
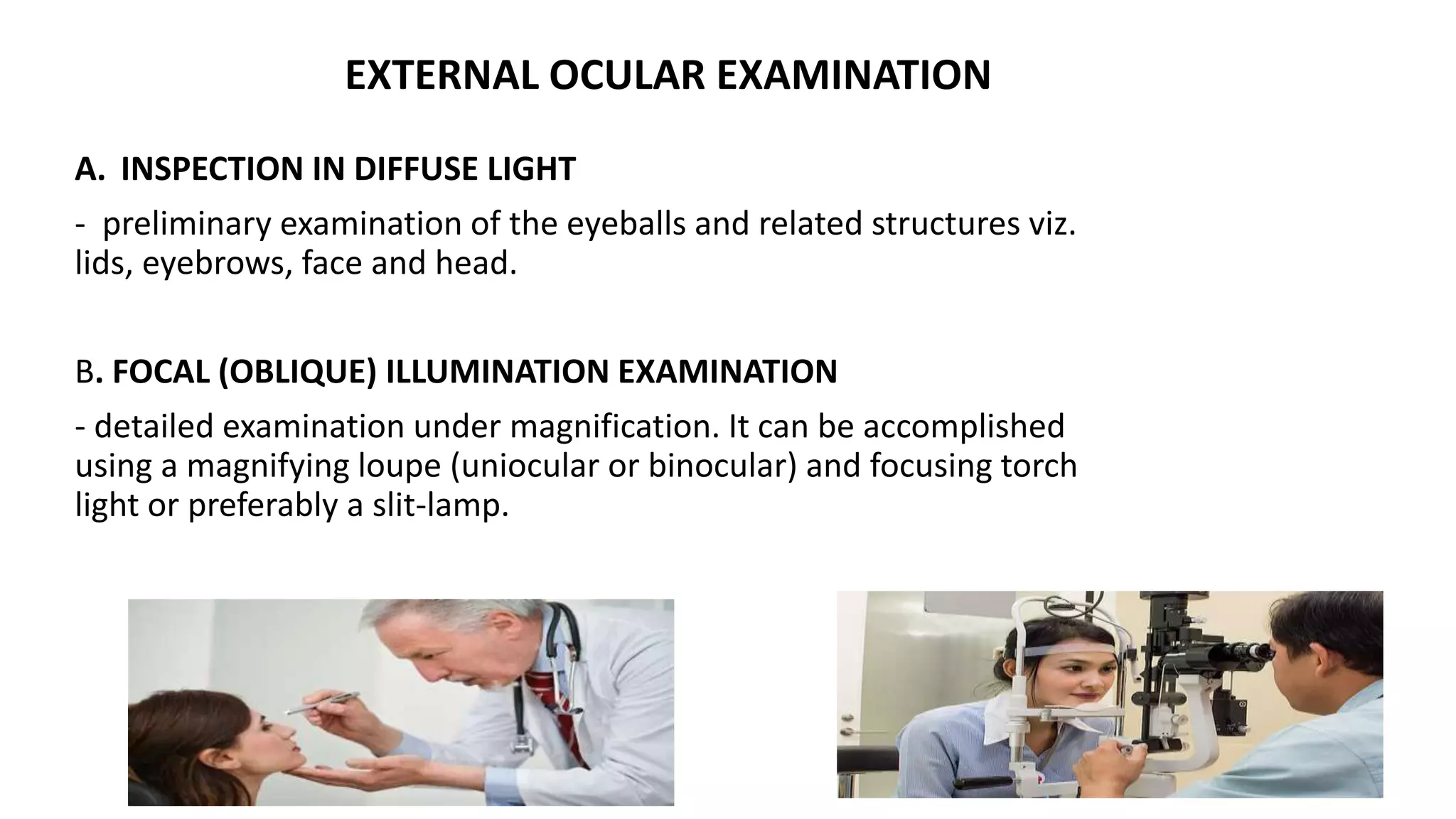
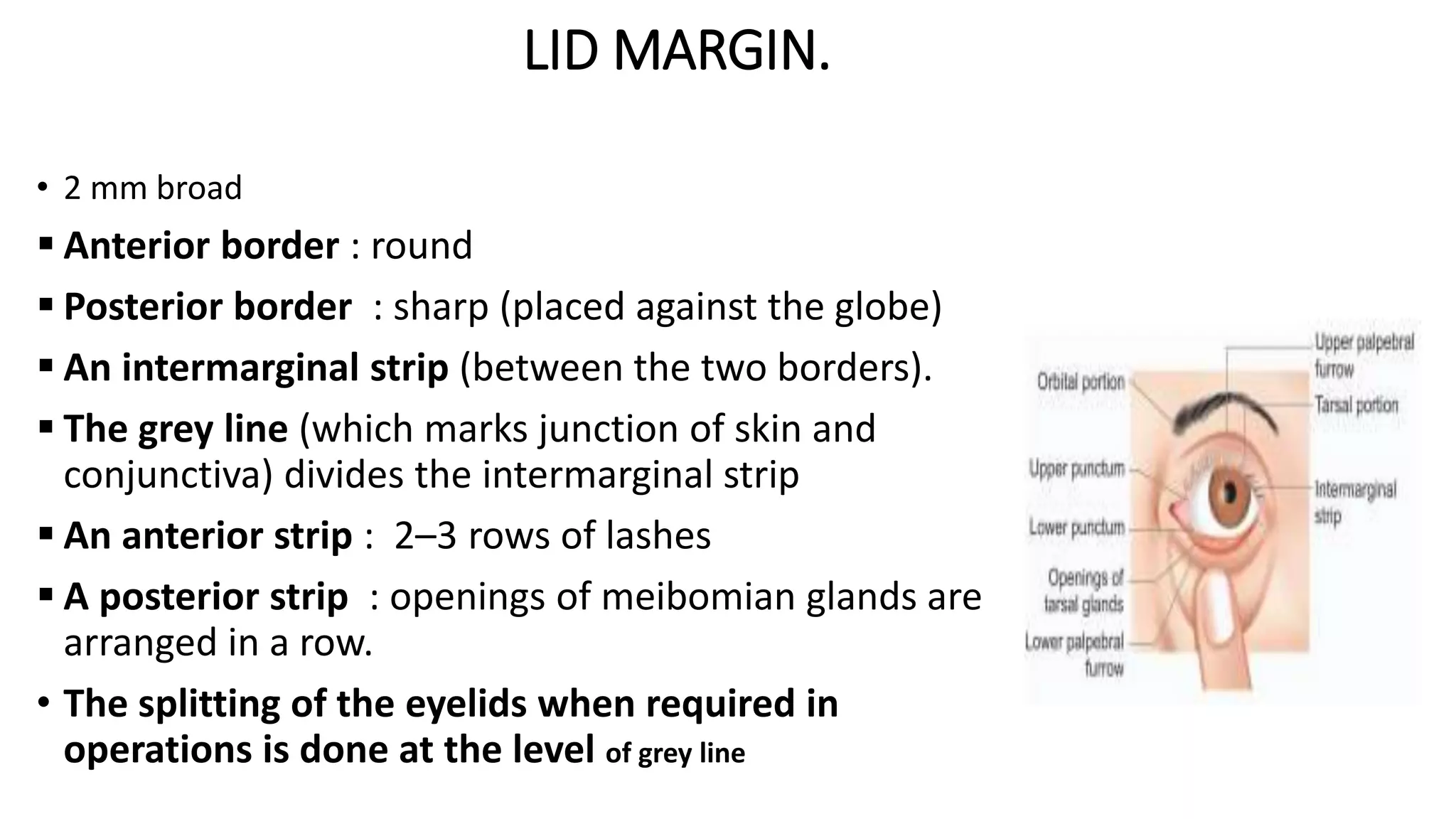
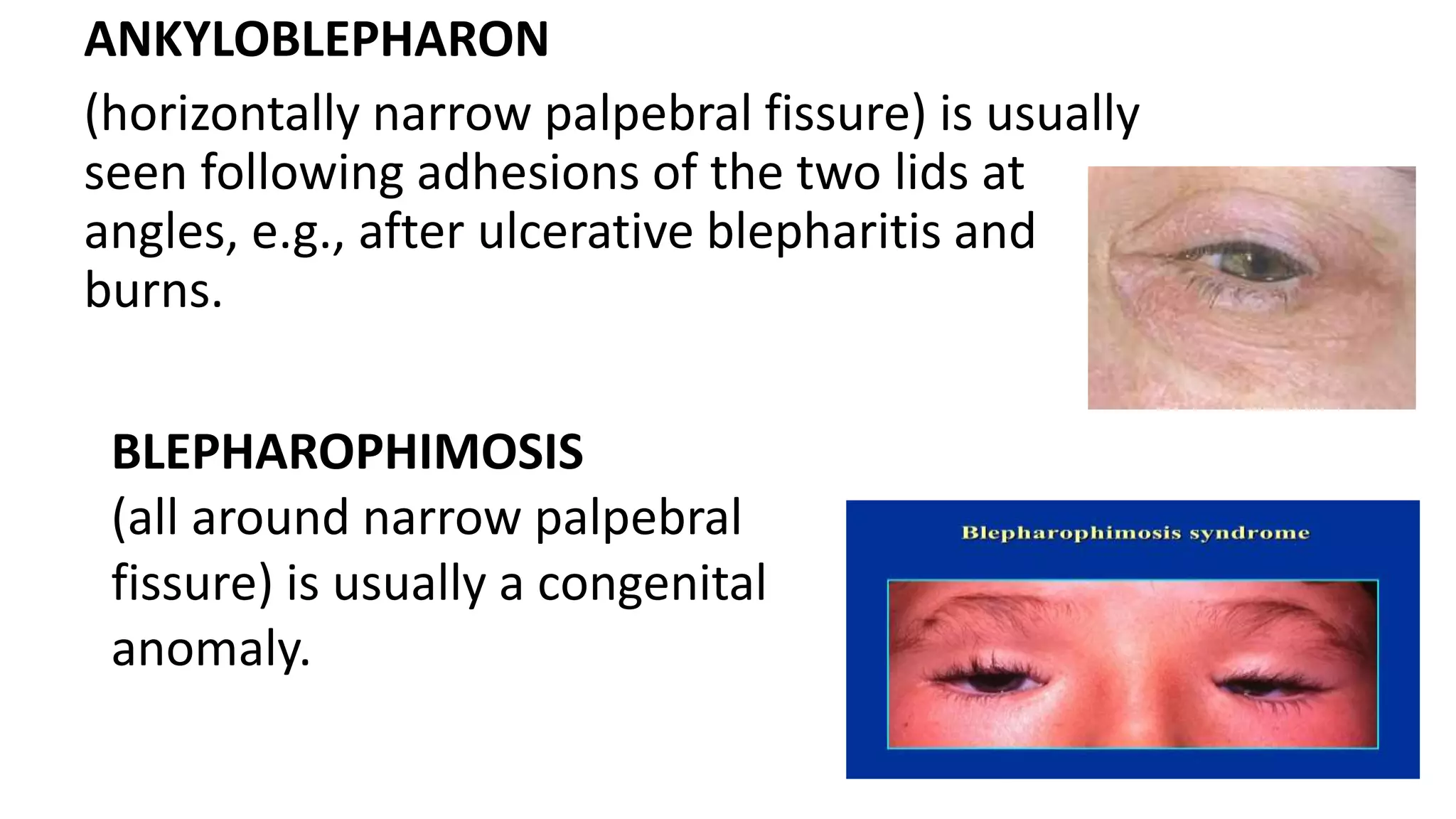
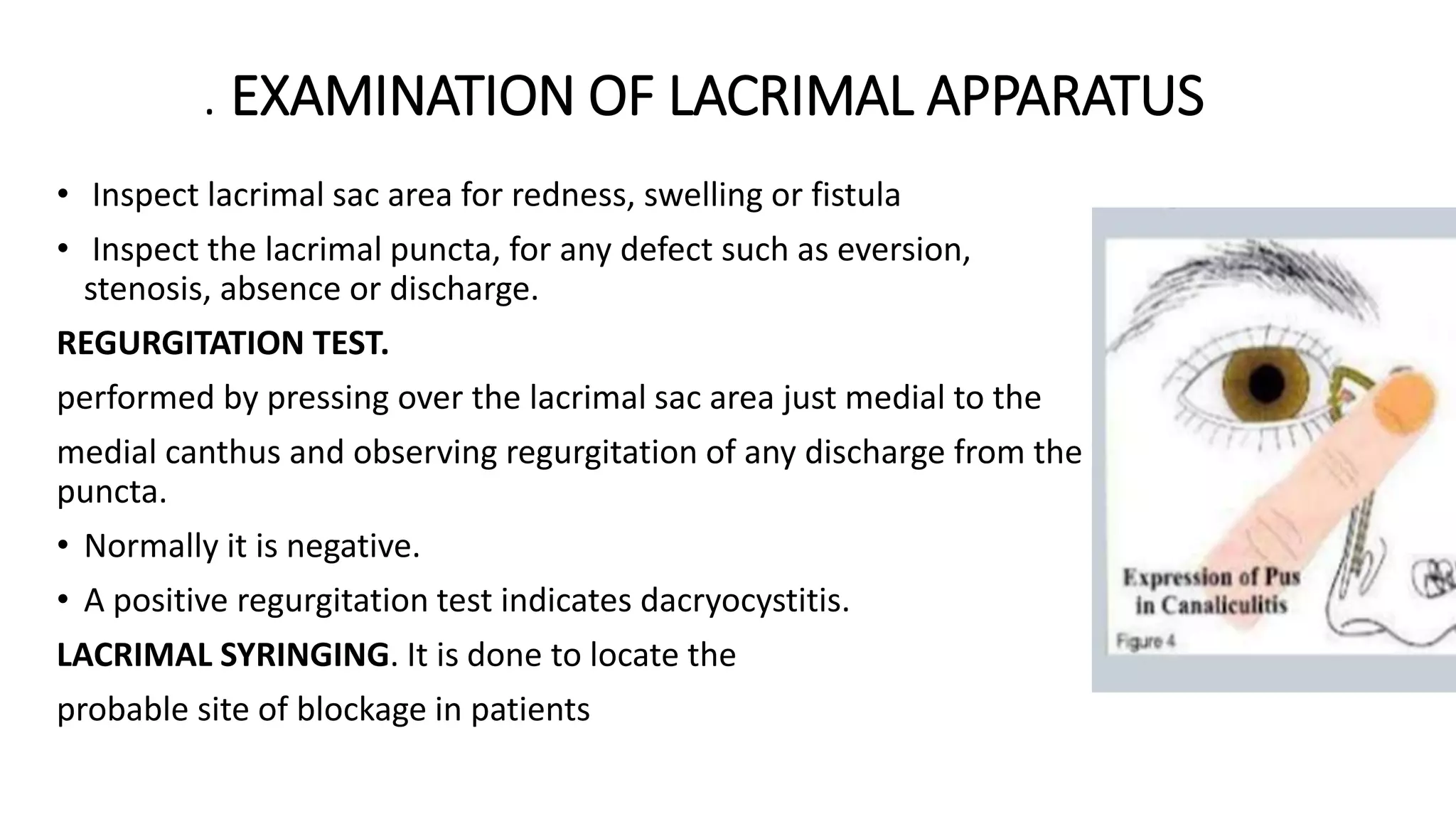
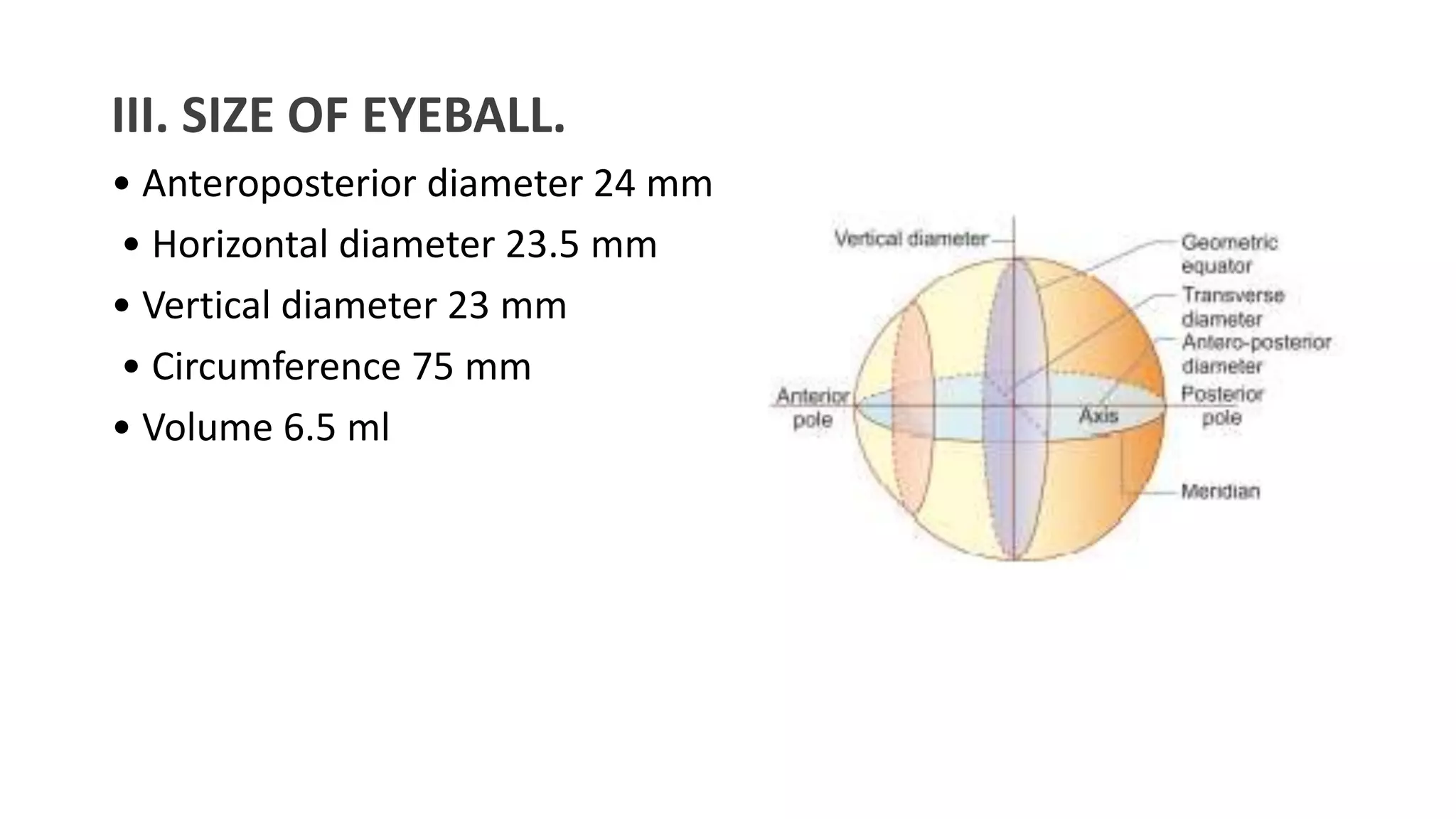
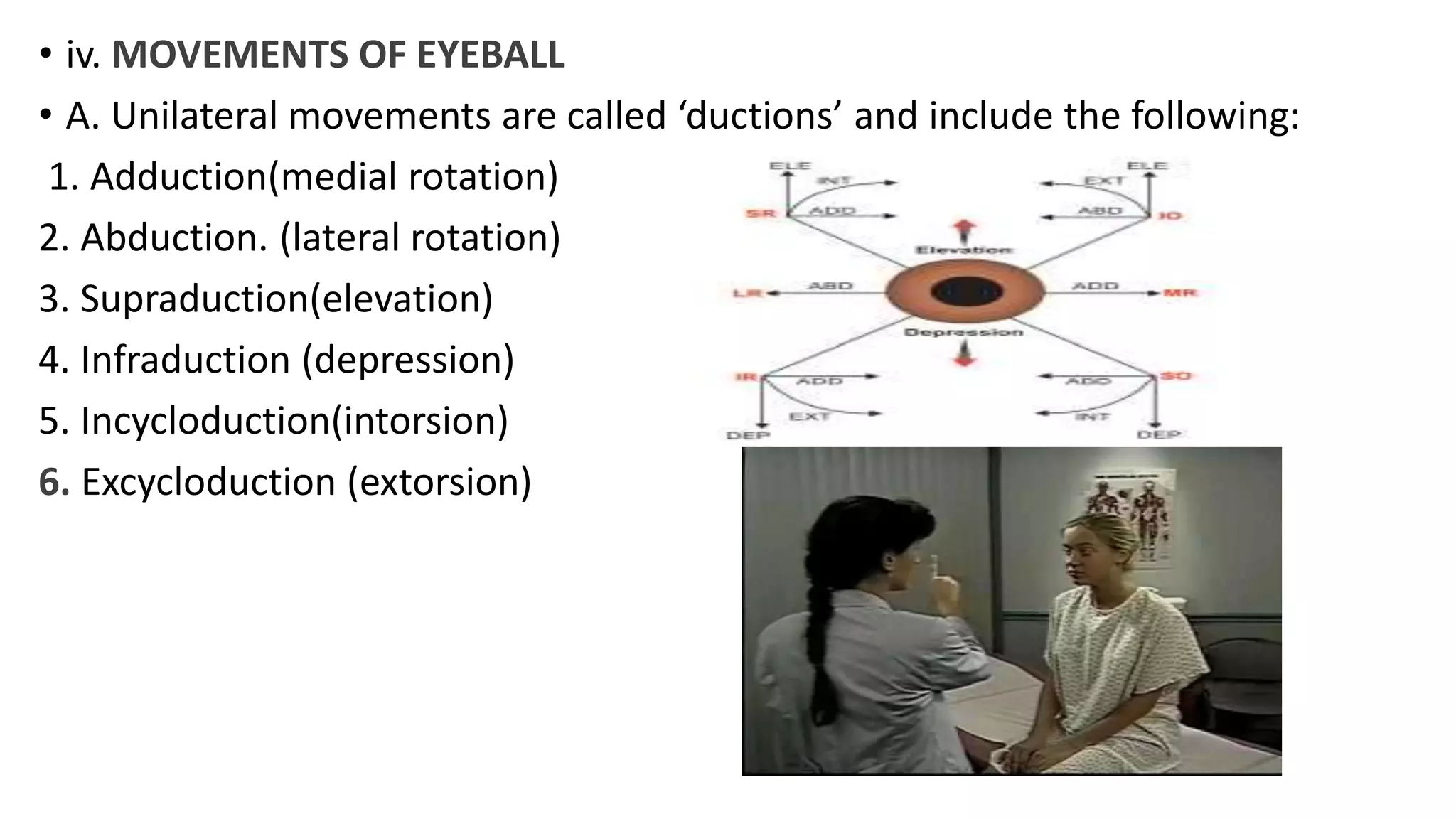
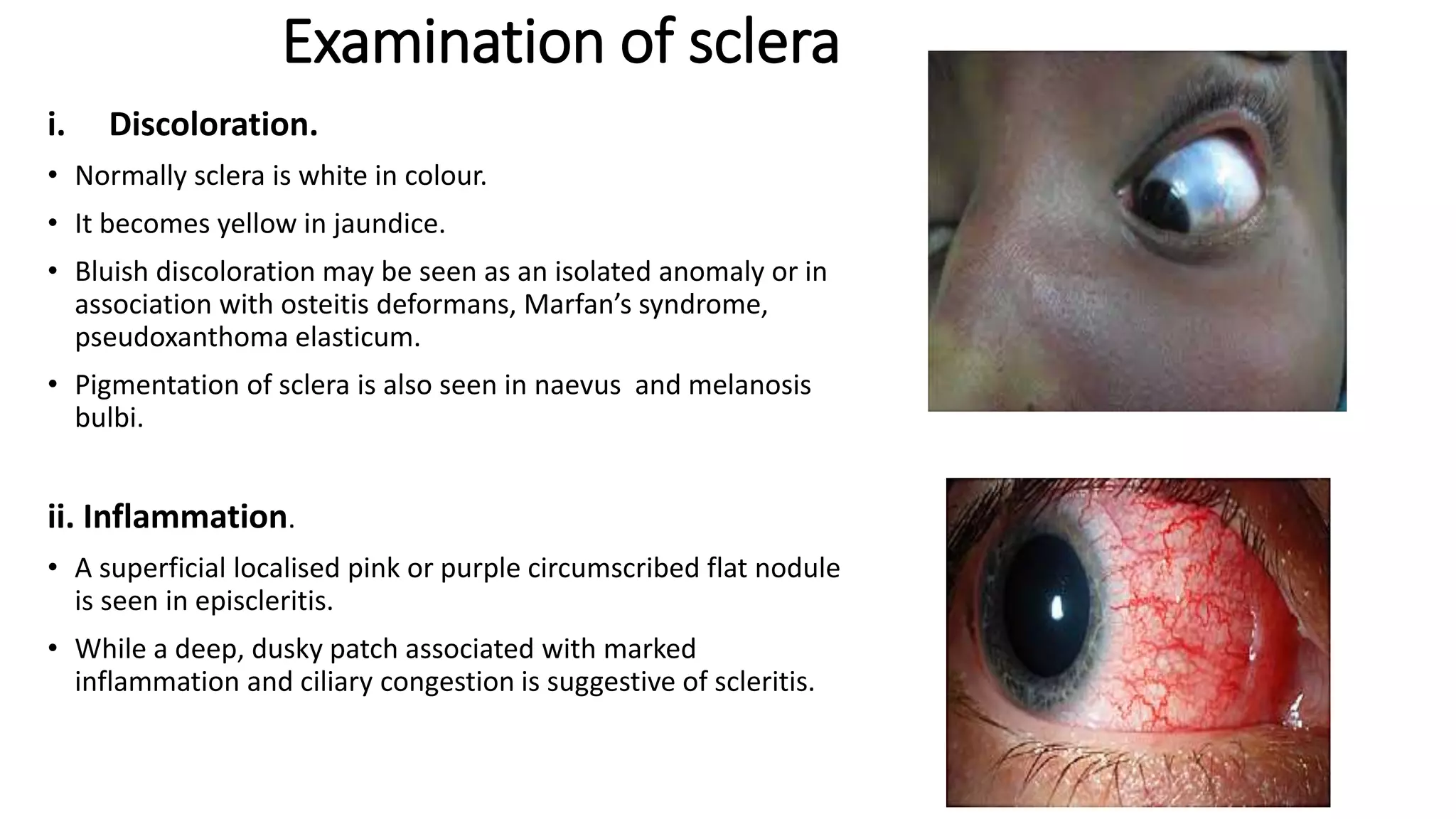
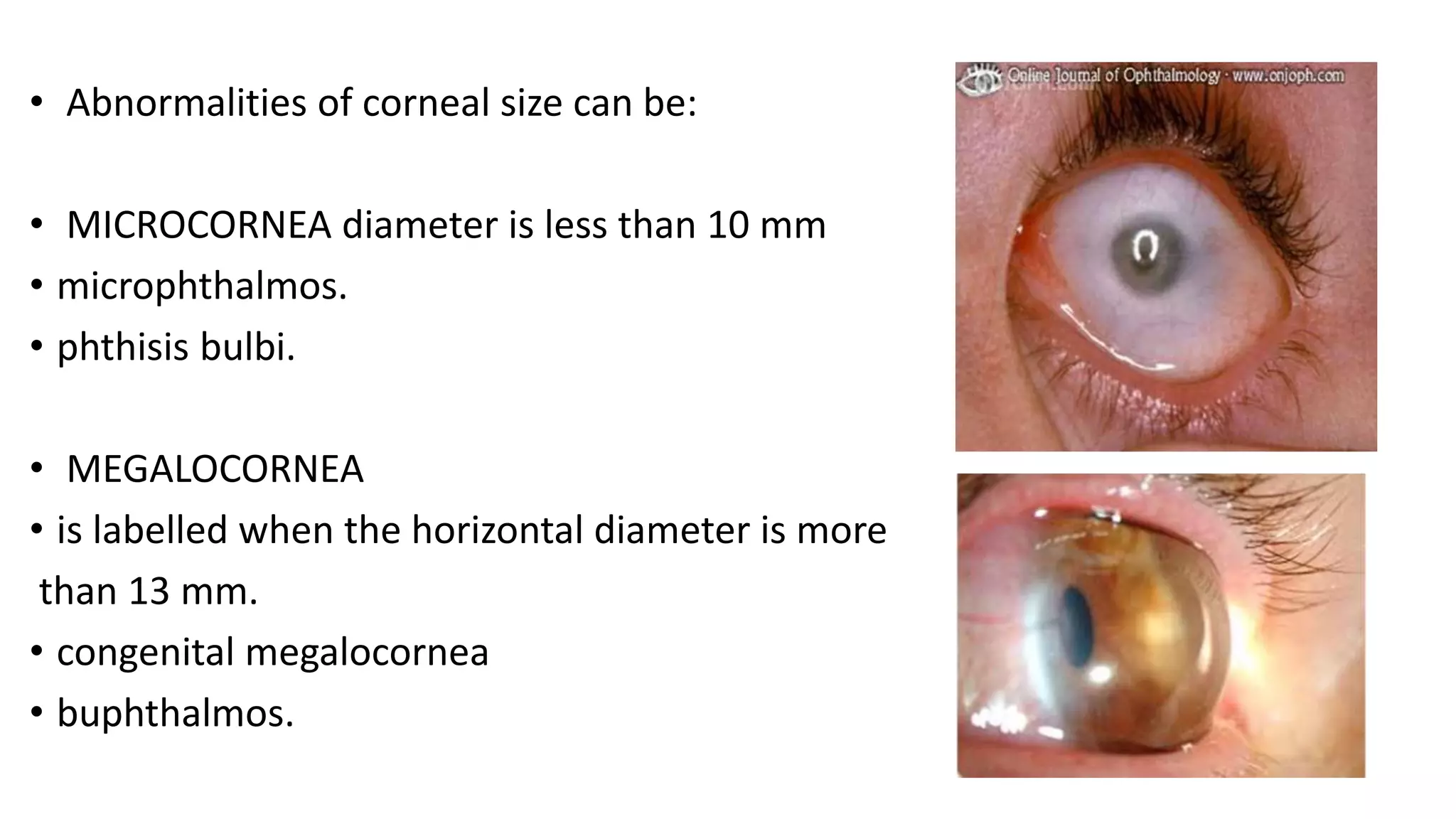
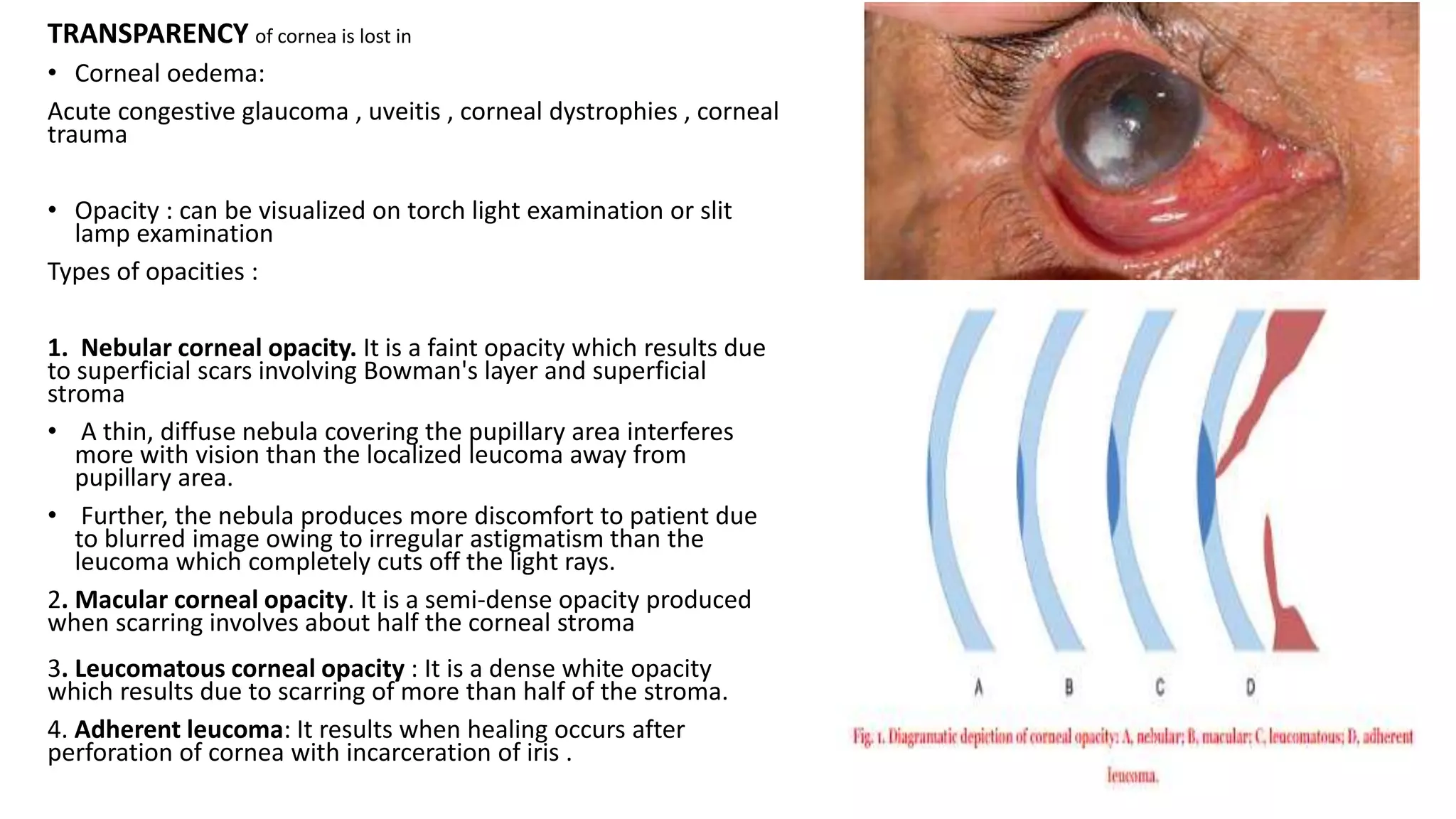
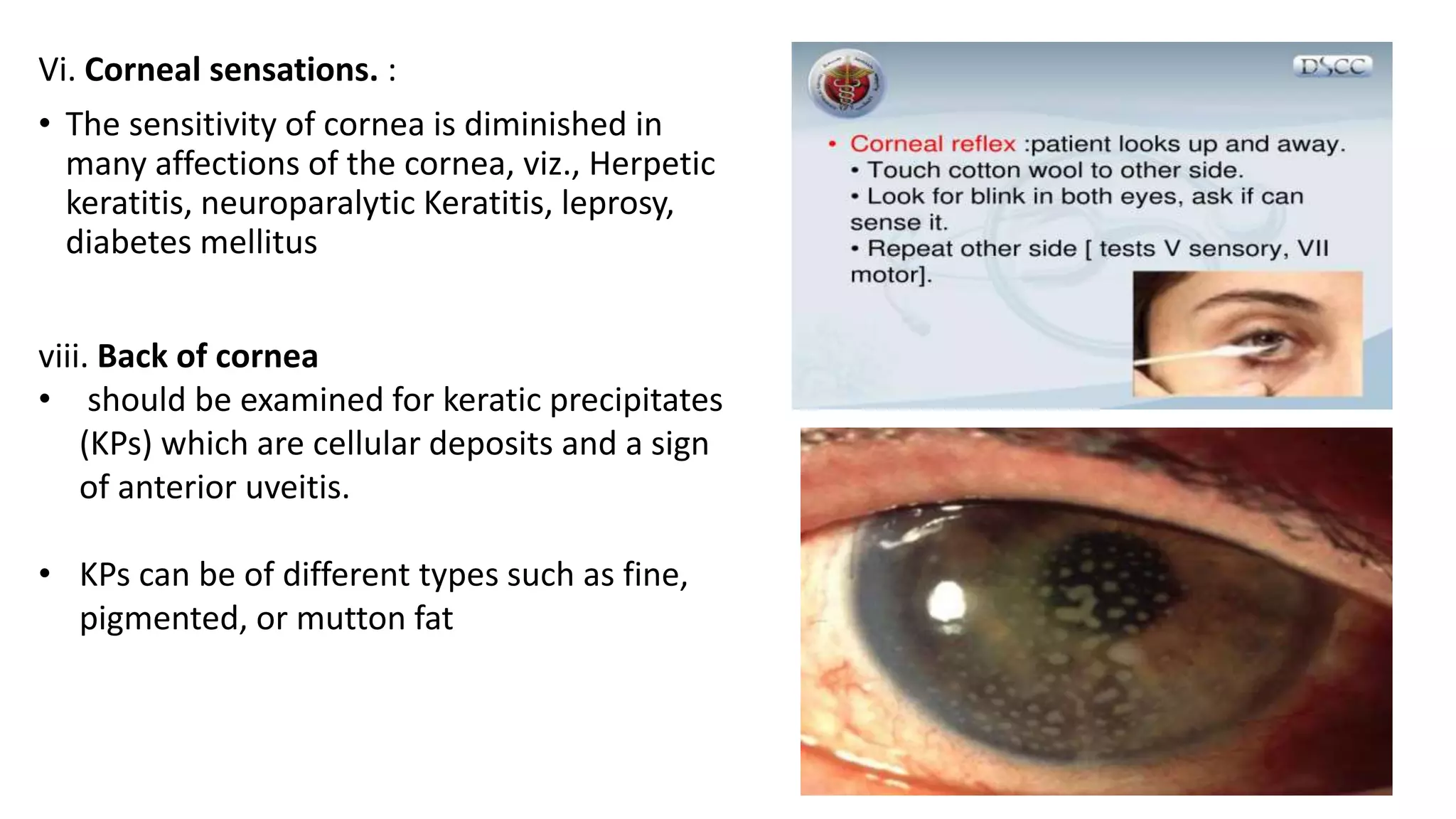
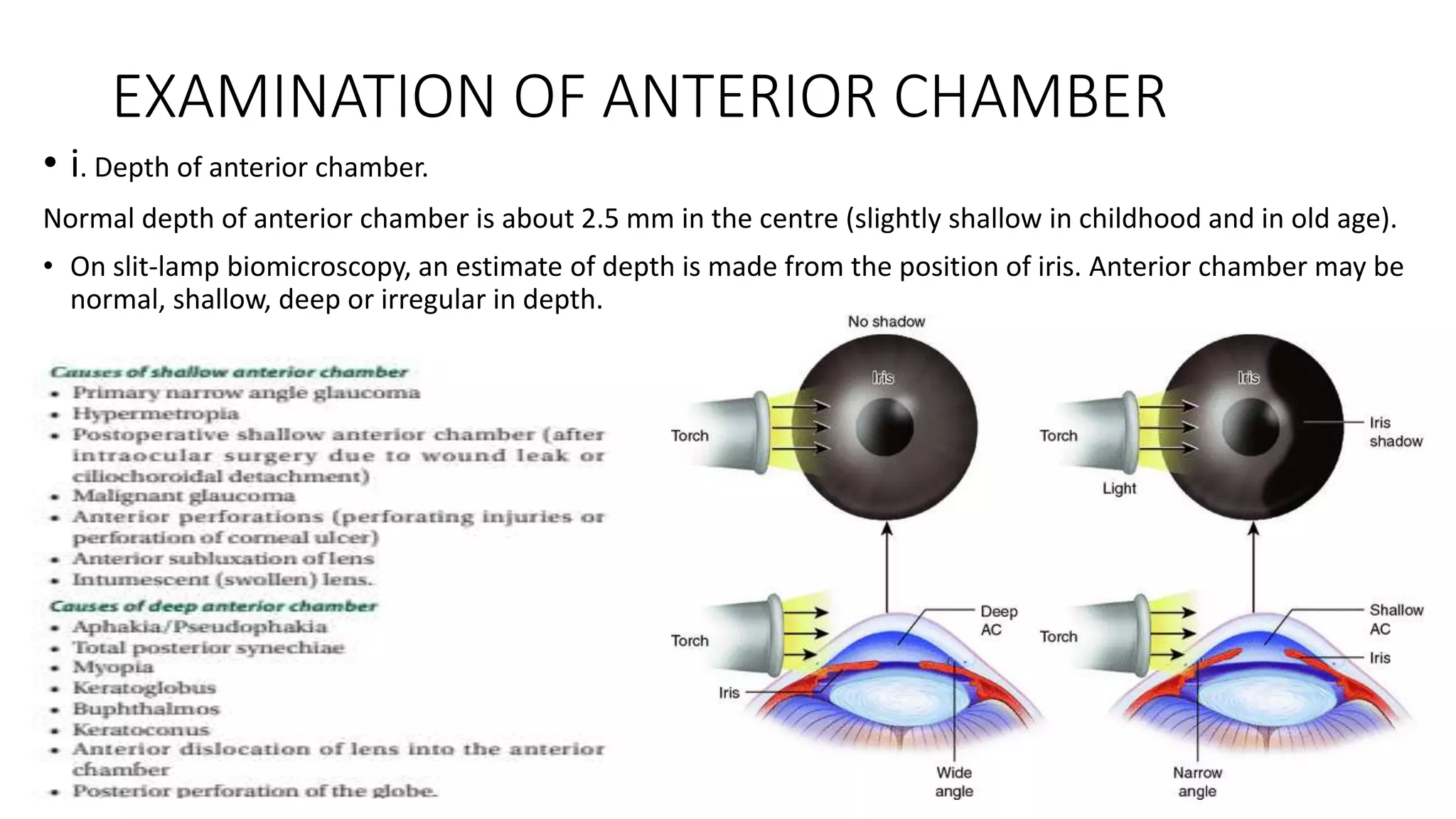
This document provides guidance on examining the eye. It describes examining the general physical health, visual function, visual acuity, external structures like eyelids and lacrimal apparatus, and internal structures of the eyeball. Key steps include testing visual acuity, checking extraocular movements, and examining the anterior and posterior segments with tools like a slit lamp. The document outlines examining various structures like the cornea for shape, size, transparency and ulcers. It also details assessing the anterior chamber contents and depth. A thorough eye exam evaluates both external and internal eye health and function.