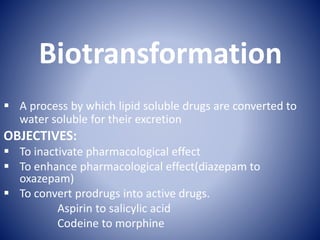
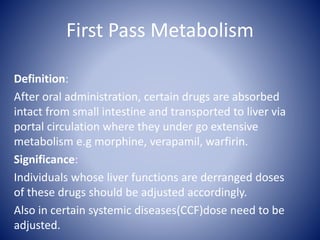
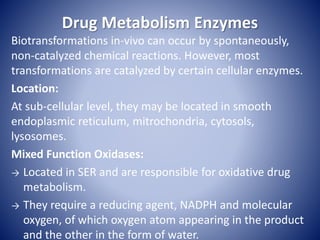
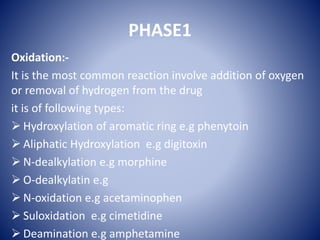
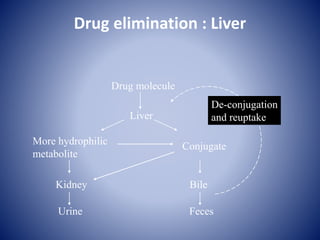
Biotransformation is the process by which lipid soluble drugs are converted to water soluble metabolites for excretion. The objectives are to inactivate drugs, enhance effects, or convert prodrugs to active drugs. The major sites are the liver, intestines, stomach, blood, brain, kidneys, and lungs. First pass metabolism occurs when orally administered drugs are absorbed and transported to the liver where they undergo extensive metabolism before reaching systemic circulation. Drug metabolism enzymes, especially cytochrome P450 enzymes in the liver, catalyze biotransformations through phase I reactions like oxidation and reduction and phase II conjugation reactions. Factors like age, weight, sex, genetics, disease processes, and drug interactions can impact an individual's