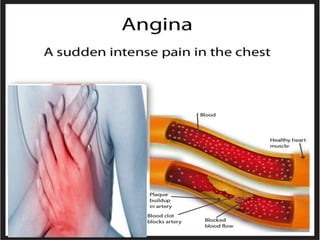
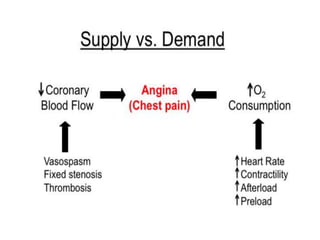
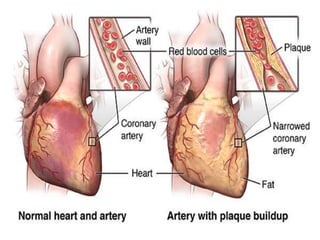
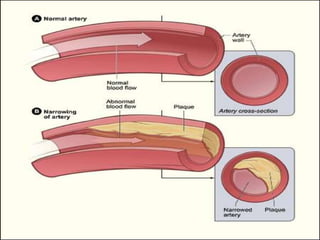
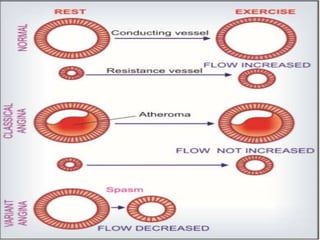
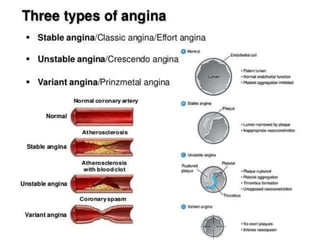
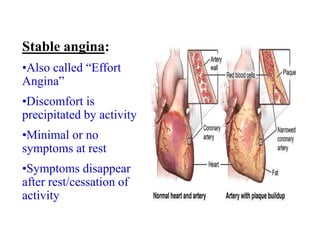
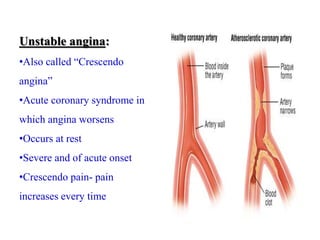
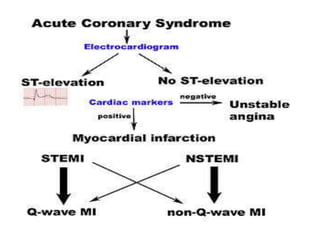
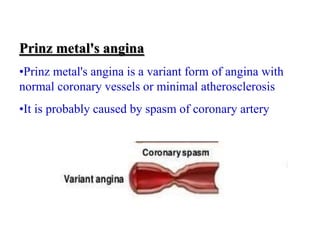
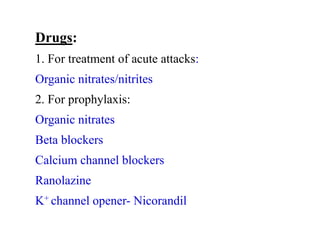
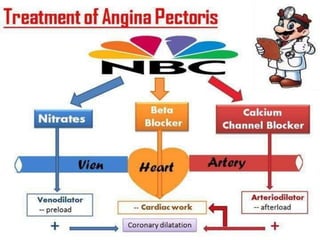
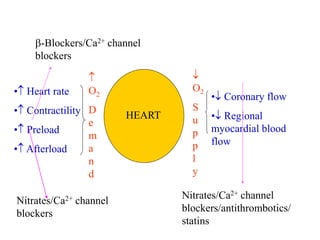
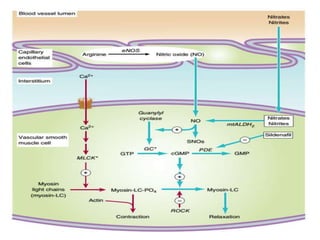
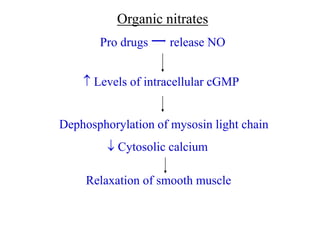
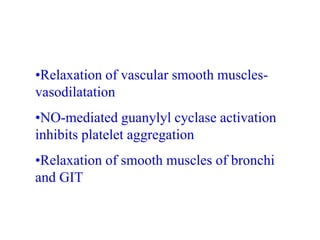
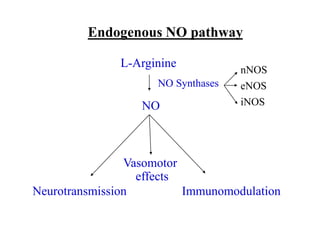
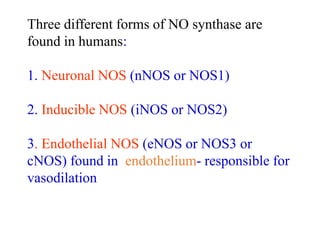
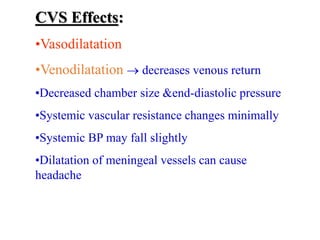
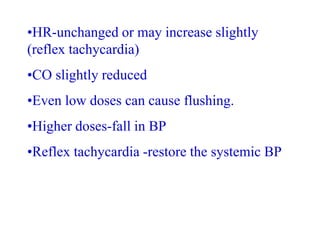
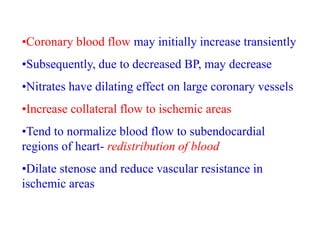
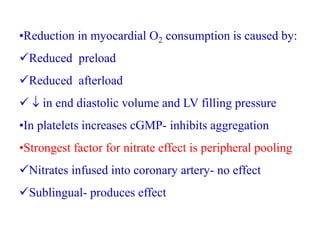
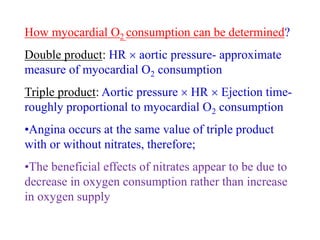
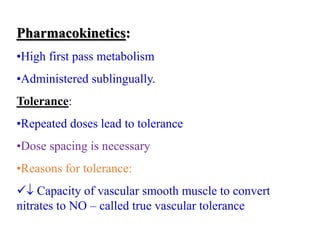
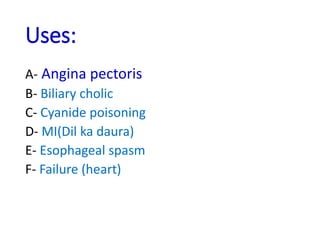
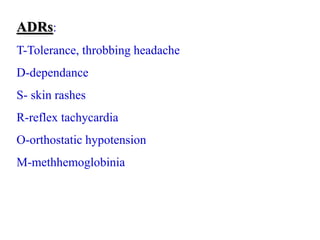
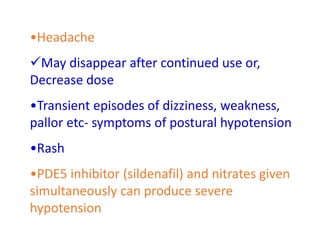
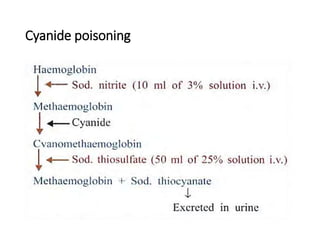
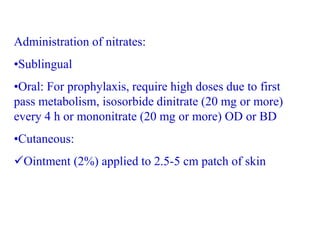
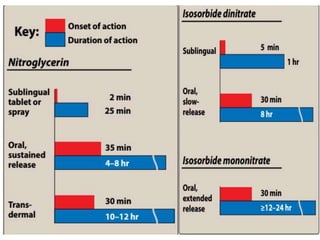
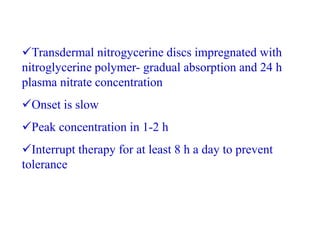
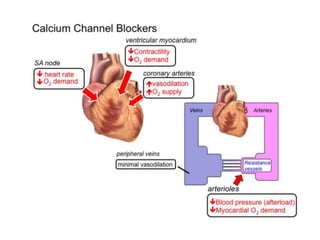
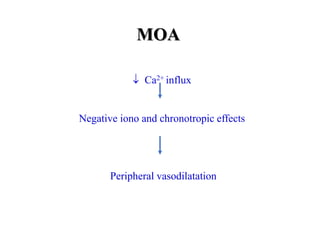
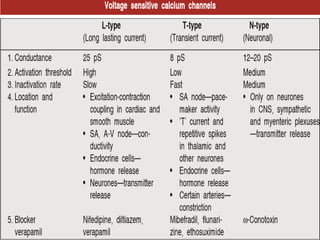
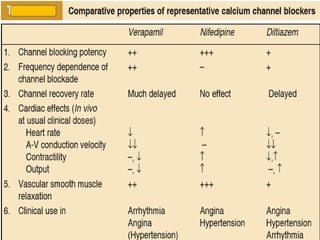
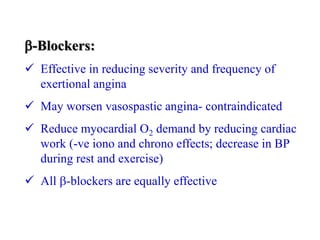
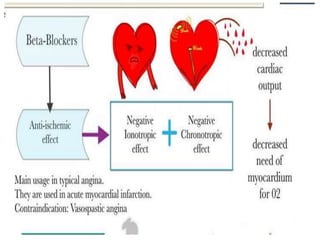
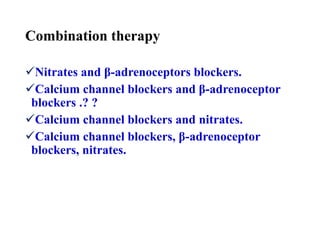
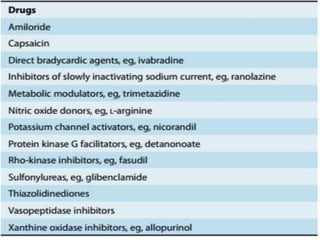
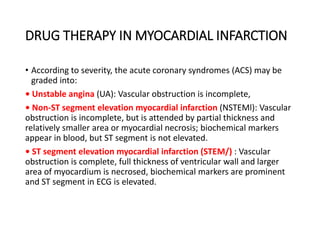
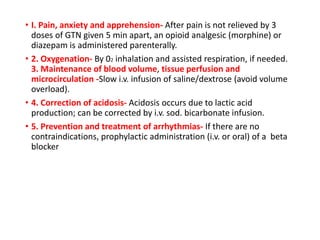
This document provides learning objectives and content on the management of ischemic heart disease. It defines stable and unstable angina, describing their underlying pathologies. It classifies drugs used to treat angina, describing the mechanisms of action, uses, and side effects of nitrates, calcium channel blockers, beta blockers, nicorandil, and ivabradine. The management of myocardial infarction is also covered, outlining treatment strategies for pain, oxygenation, hemodynamics, arrhythmias, and use of antiplatelet/anticoagulant drugs and thrombolysis.