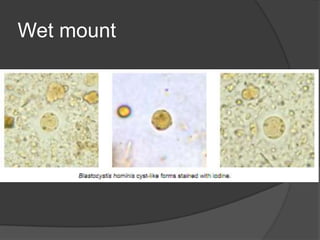
Blastocystis hominis is a common intestinal parasite that infects humans. It was originally classified as a yeast but is now known to lack a cell wall. It reproduces by binary fission or sporulation under anaerobic conditions. Symptoms of blastocystosis include diarrhea, abdominal pain, and nausea. Diagnosis involves microscopic examination of stool samples. Treatment is with metronidazole or other antibiotics. Prevention involves safe drinking water and basic sanitation practices.