This document discusses peripheral artery disease (PAD), including:
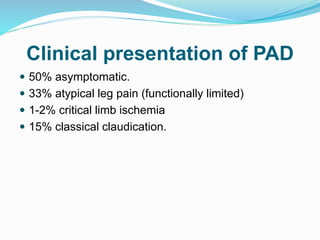
- PAD affects over 200 million people worldwide and causes intermittent claudication in 5% of men and 2.5% of women.
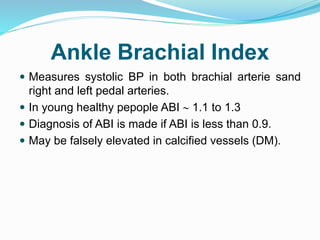
- Patients at highest risk include those over 65, males, diabetics, smokers, and those with an ankle-brachial index over 0.9.
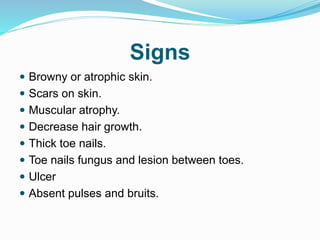
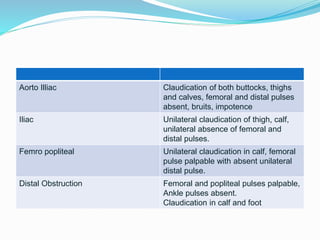
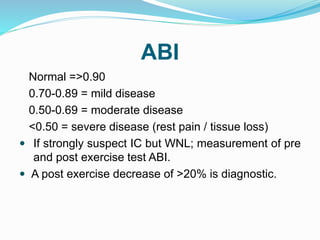
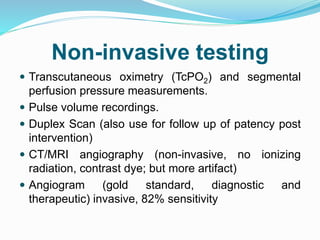
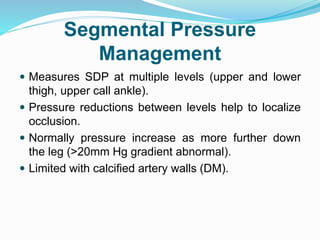
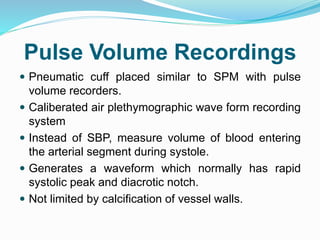
- Diagnosis involves history, physical exam including pulse checks, ankle-brachial index, and tests like duplex ultrasound, angiography.
- Treatment involves risk factor modification, exercise, medications like cilostazol, and referral for revascularization for severe or critical limb ischemia.