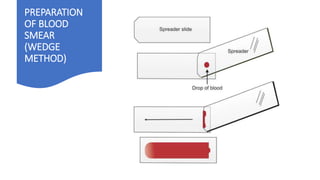
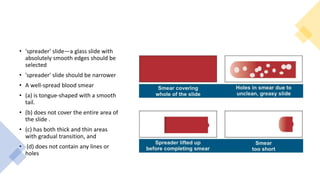
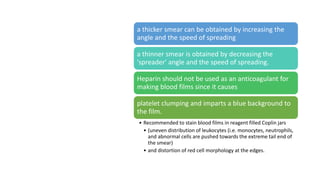
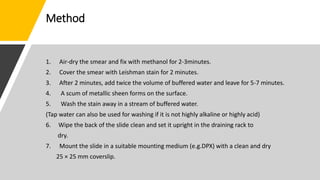
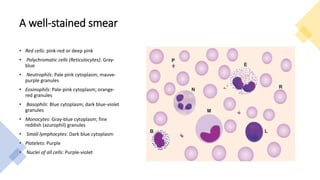
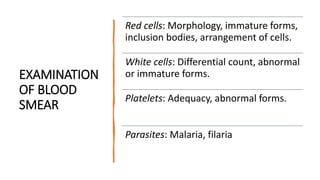
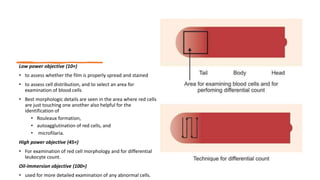
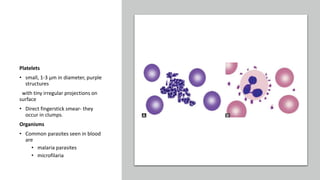
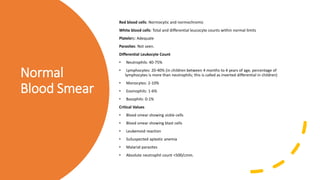
The blood smear document defines a blood smear, outlines its uses in diagnosing conditions like anemia and infections, and provides detailed instructions on preparing, staining, examining, and interpreting a blood smear slide. A well-prepared blood smear shows red and white blood cells with normal morphology, and is examined under microscopy to check for abnormalities and identify blood parasites or immature cells that can indicate conditions like infection or leukemia.