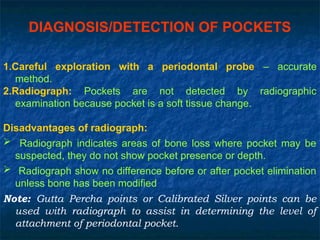
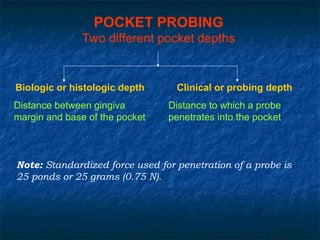
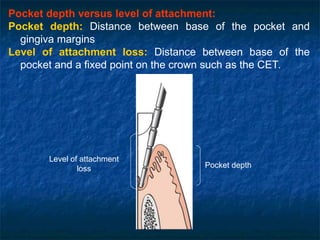
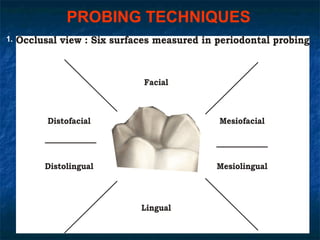
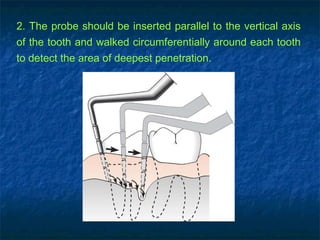
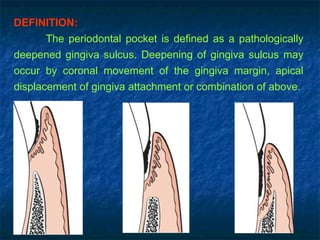
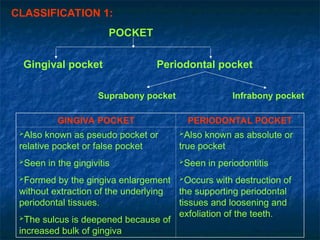
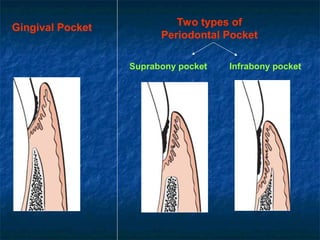
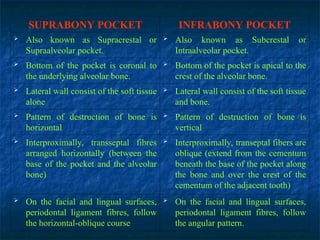
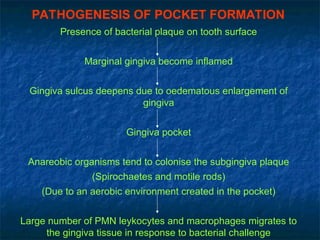
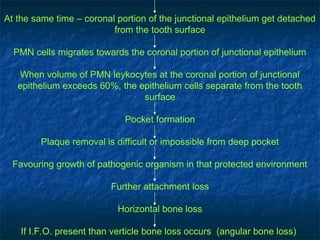
A periodontal pocket is a deepened gingival sulcus resulting from apical displacement of the gingival attachment or coronal movement of the gingival margin, associated with conditions like gingivitis or periodontitis. The document categorizes pockets into types based on their characteristics and origins, discussing their clinical features, pathogenesis, and histopathology, as well as methods for diagnosis and probing techniques. It emphasizes the continuous inflammatory nature of these pockets and the challenges in their treatment due to plaque accumulation and bacterial presence.
![HISTOPATHOLOGY
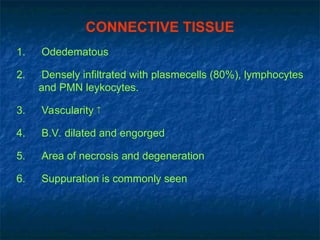
[I] Soft tissue wall/lateral wall
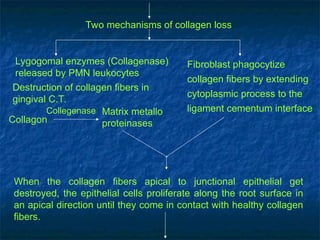
Epithelium:
Shows
1. Epithelial cells proliferate into the underlying connective
tissues forming deep rete pegs
2. Micro ulcerations develops on soft tissue wall
3. Pocket epithelial is infiltrated by PMN’s and oedematons fluid
from inflammed connective tissues.
4. Bacterial invasion in intercellular space of epithelium (eg.
Gram negative organism, porphysomons gingivais, provotella
intermedia, actinobacillus).
Degenerative changes
Proliferative changes](https://image.slidesharecdn.com/peridontal-pocket-perio-241101172300-ac9248f7/85/Peridontal-Pocket-Perio-study-guide-exam-12-320.jpg)
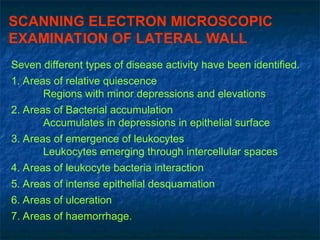
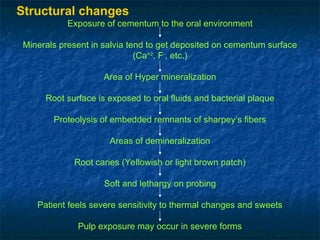
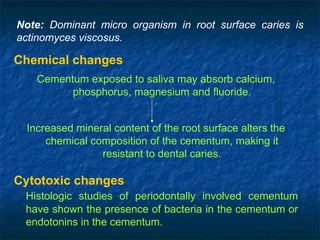
![[II] Root surface wall of the pocket
Root surface forms the medial wall of the pocket.
The root surface that gets expose to the oral
environment, as a result of periodontal attachment loss,
undergoes following changes.
Structural changes Chemical changes Cytotonic changes](https://image.slidesharecdn.com/peridontal-pocket-perio-241101172300-ac9248f7/85/Peridontal-Pocket-Perio-study-guide-exam-17-320.jpg)