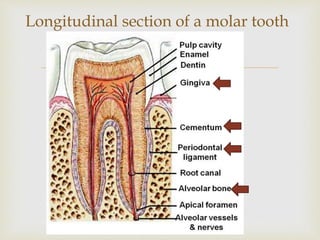
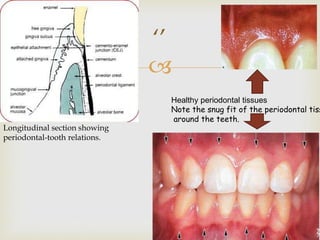
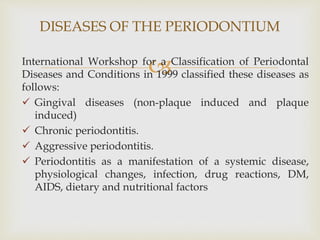
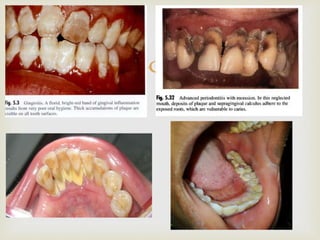
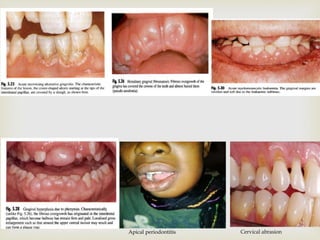
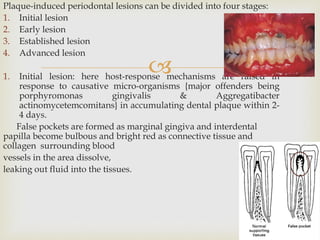
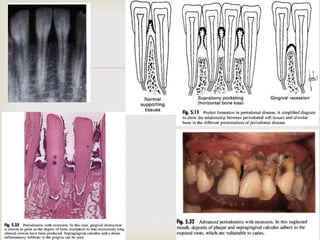
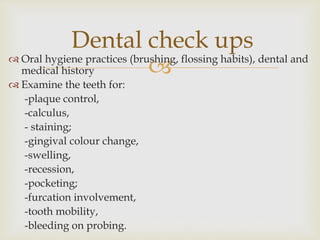
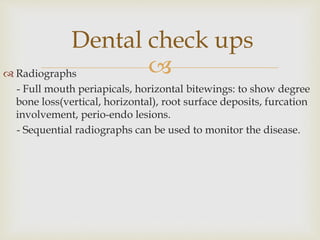
The document discusses periodontal diseases, which affect the tissues that surround and support teeth. It defines the periodontium and periodontal diseases. The most common periodontal diseases are gingivitis and periodontitis. Gingivitis is inflammation of the gums caused by plaque buildup. Periodontitis is a more advanced form involving loss of bone and tissues that support the teeth. The document outlines the classification, causes, pathogenesis, clinical presentation, and management of periodontal diseases. Effective treatment requires eliminating plaque and other contributing factors, followed by corrective procedures and long-term maintenance.