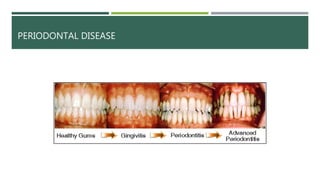
This document provides an overview of periodontal disease, including the periodontal team, causes, symptoms, classifications, diagnostic procedures, and treatments. The main points are:
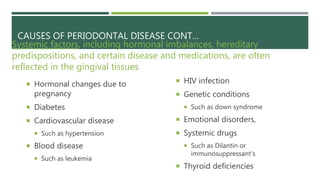
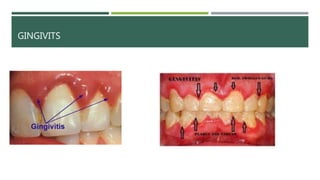
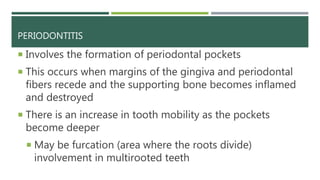
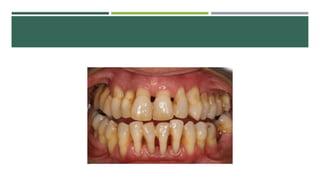
- Periodontal disease involves inflammation and infection of the gums and bone around the teeth. It is common and can be caused by plaque, calculus, poor oral hygiene, and certain medical conditions.
- The periodontal team includes the periodontist, dental assistants, hygienists, and office staff who work together to treat and manage periodontal disease.
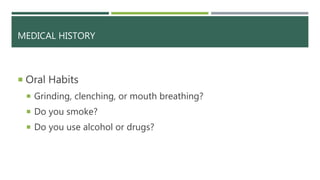
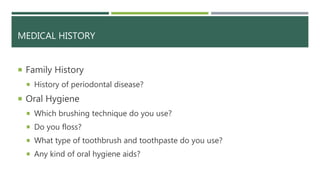
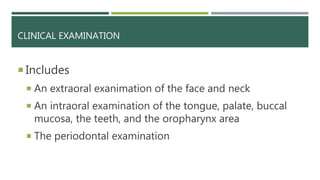
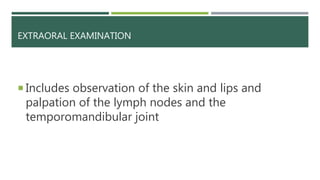
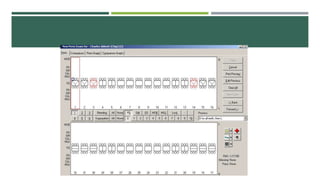
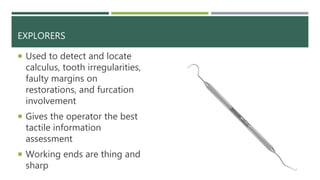
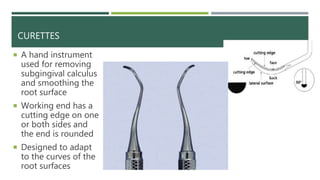
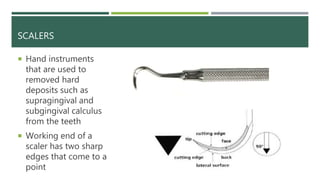
- Diagnostic procedures include a medical history, examination, x-rays, and periodontal screening to assess the patient's condition and develop a treatment plan.