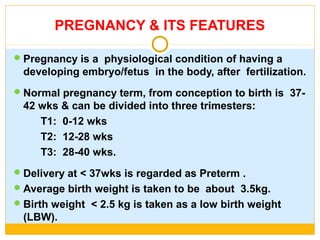
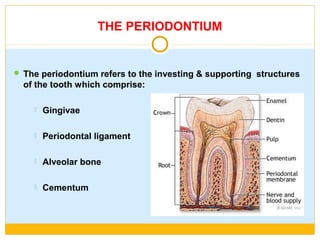
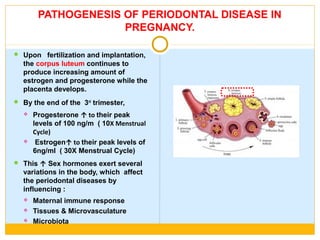
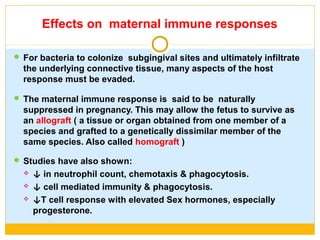
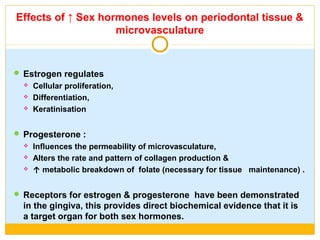
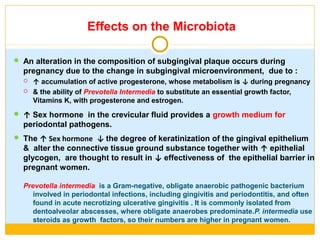
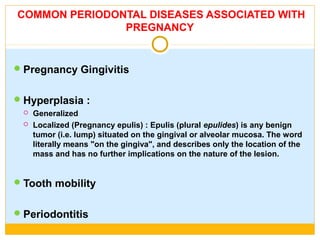
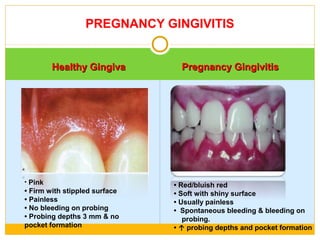
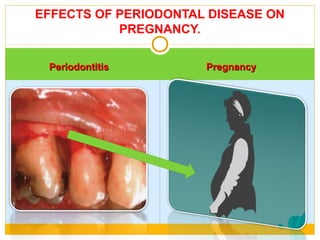
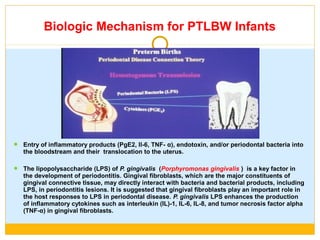
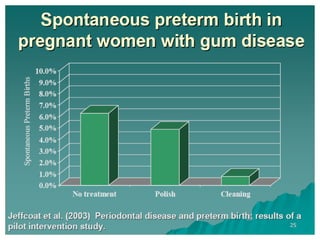
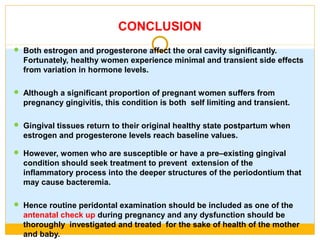
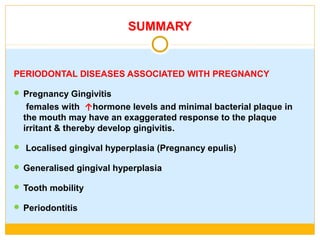
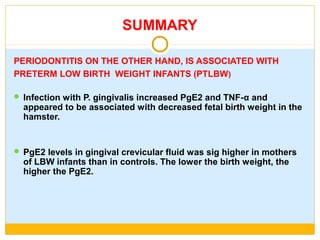
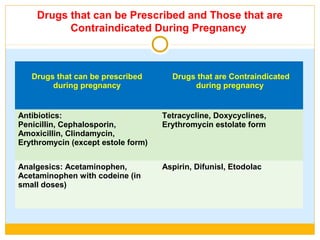
The document discusses the effects of pregnancy on periodontal health. It notes that pregnancy causes physiological changes that can impact the periodontium, including increased sex hormone levels. This can suppress the immune response and alter the tissues, microvasculature, and microbiota in the mouth. Common periodontal issues in pregnancy include gingivitis, hyperplasia, tooth mobility, and periodontitis. Untreated periodontal disease is identified as a potential risk factor for preterm birth and low birthweight babies. The document recommends preventative measures like nutrition, supplements, and good oral hygiene to maintain periodontal health during pregnancy.