This document discusses pediatric contact lens management and fitting considerations. Key points include:
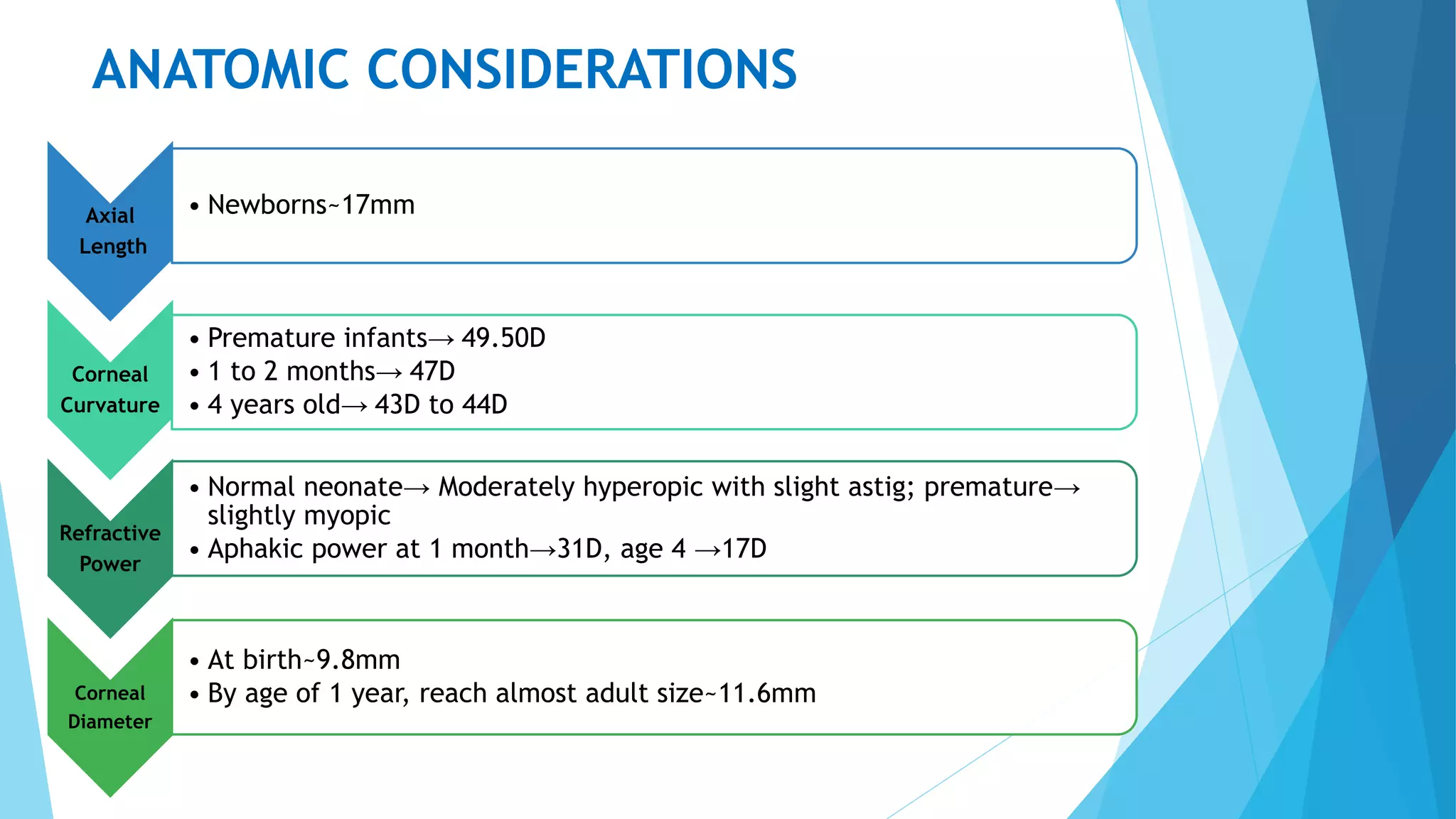
- Anatomical considerations for pediatric eyes such as shorter axial length and steeper corneal curvature compared to adults.
- Indications for pediatric contact lens fitting include high refractive errors, aphakia, and irregular astigmatism.
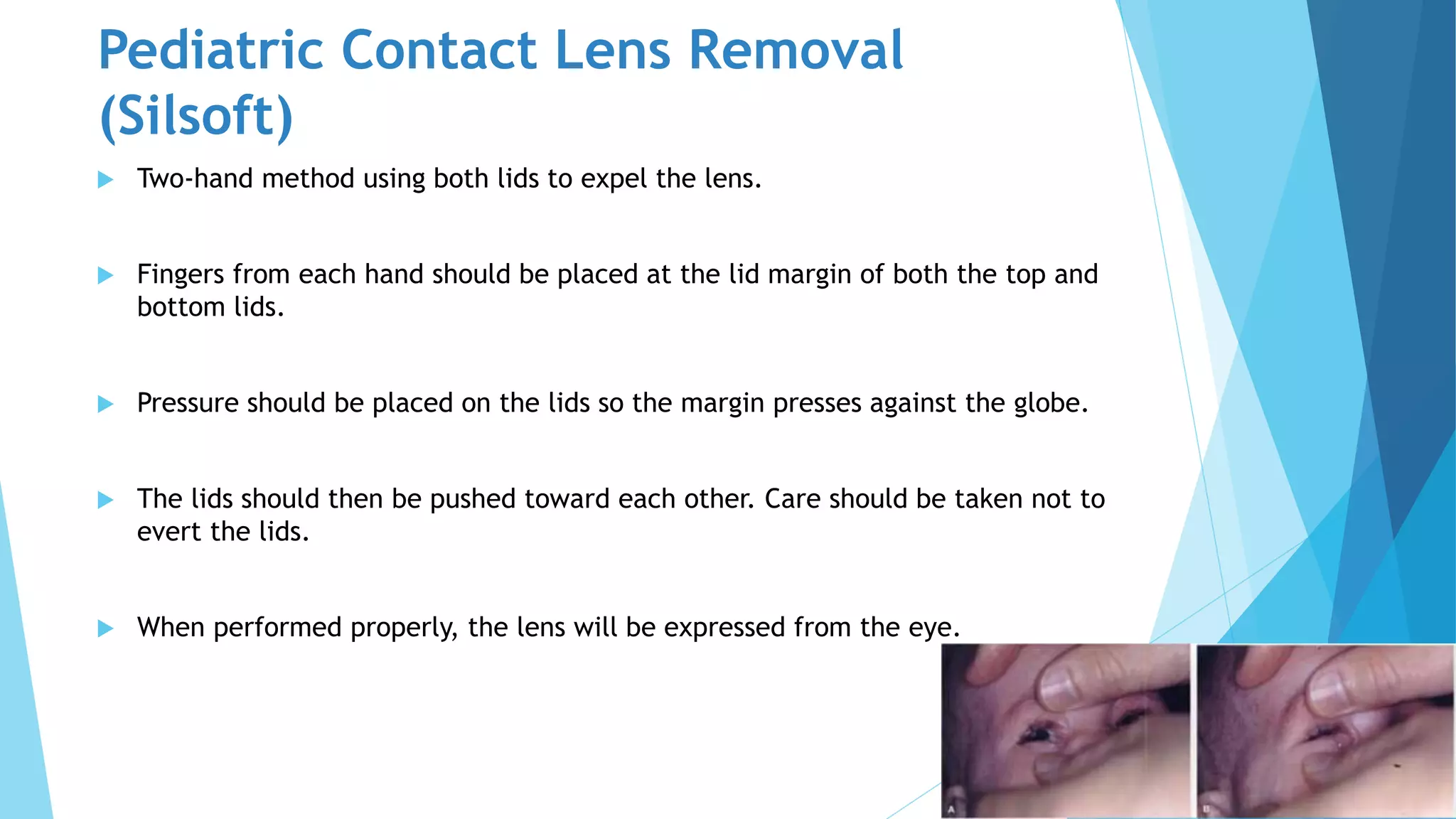
- Silicone elastomer, hydrogel, and RGP lenses are commonly used in pediatric fittings, each with advantages and disadvantages.
- A thorough prefitting exam evaluates lid and corneal health before determining initial lens parameters based on age.
- Fitting is assessed using fluorescein pattern and lens movement, with progress evaluated regularly according to age.