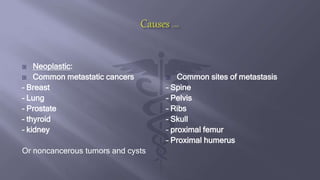
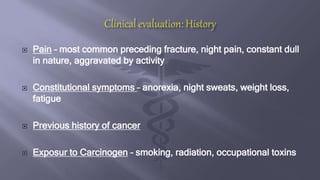
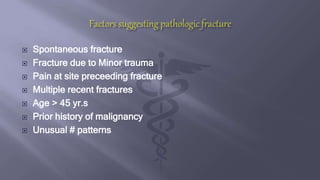
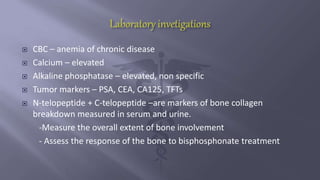
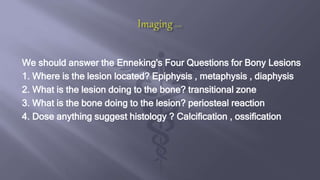
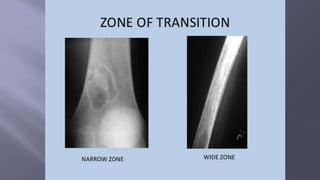
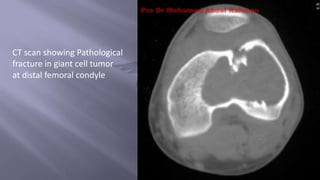
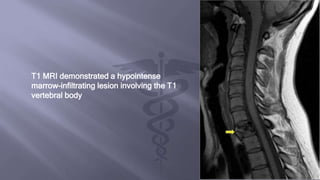
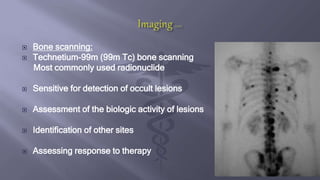
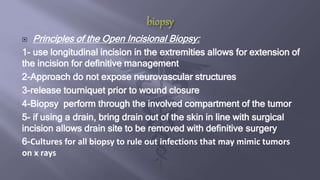
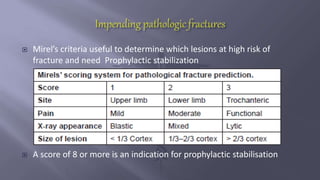
Pathological fractures occur through an abnormal focal area of bone, which can be malignant or non-malignant. Common sites of bone metastases that cause pathological fractures are the spine, pelvis, ribs, skull, proximal femur and humerus. Diagnosis involves imaging like x-rays, CT, MRI and bone scans to identify the fracture line and assess the extent of involvement. Treatment depends on factors like life expectancy, severity of symptoms, and includes options like bracing, radiation, bisphosphonates, or surgery to stabilize and relieve pain. The goals of surgical treatment are early stabilization to improve function and survival.