The document provides a comprehensive overview of acute heart failure, including its definition, classification, causes, and epidemiology. It details triage findings, primary and secondary survey findings, diagnostic investigations, and management strategies for acute heart failure. Additionally, the document emphasizes the importance of monitoring parameters, goals of treatment, and patient disposition in clinical practice.

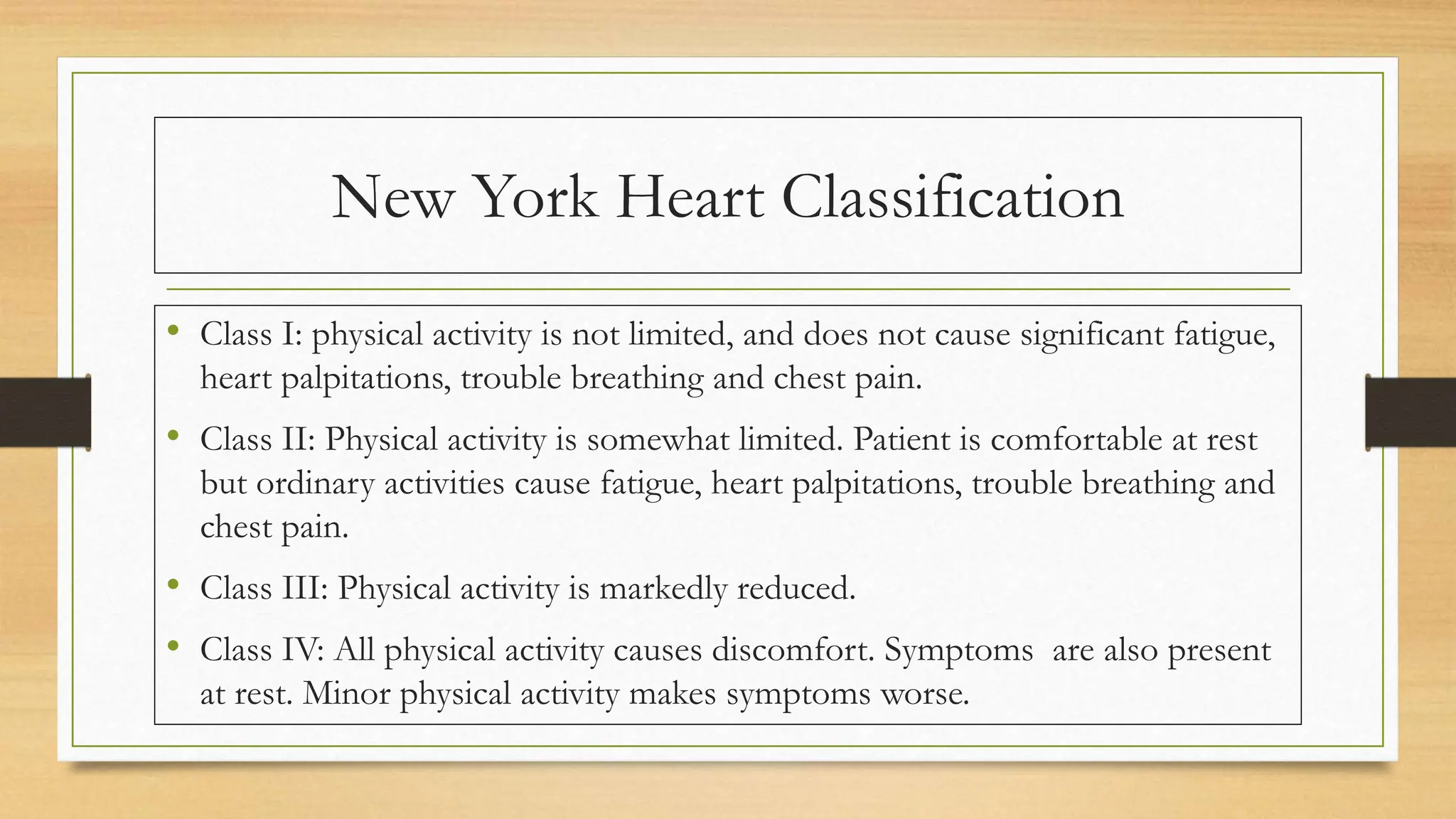



![Epidemiology in
Africa [1,2]
• In SSA, HF occurs at a young age
• Common causes of AHF include hypertensive heart disease ( 39.2%),
cardiomyopathy, (21.4%), rheumatic heart disease( 14.1%), HIV- associated
cardiomyopathy, turberculous pericardial disease, Corpulmonale and
peripartum cardiomyopathy.
• HF with systolic dysfunction is the commonest
• Hospital case fatality rates ranges 9%-12.5%.](https://image.slidesharecdn.com/acuteheartfailure2-240507180125-92eee0d7/75/Acute-Heart-Failure-presentation-by-Dr-Chikondi-Malobe-12-2048.jpg)