1. Parvovirus B19 causes a range of clinical manifestations from asymptomatic infection to transient erythroblastopenia or aplastic crisis depending on the host's immune status and underlying medical conditions.
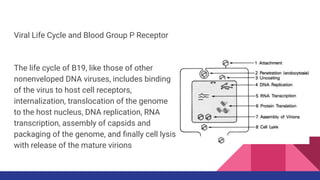
2. The virus binds to the P blood group antigen receptor on erythroid progenitor cells and causes their lysis, resulting in transient red cell aplasia. This causes a temporary anemia in healthy individuals but can cause a severe aplastic crisis in those with hemolytic anemia.
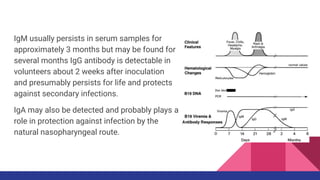
3. Diagnosis involves detecting B19 viral DNA by PCR or antibodies such as IgM, which indicates a current infection, and IgG which persists for life after infection and confers immunity.