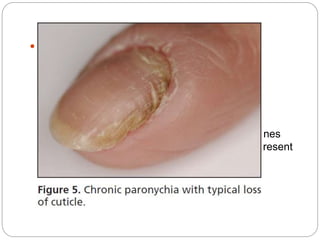
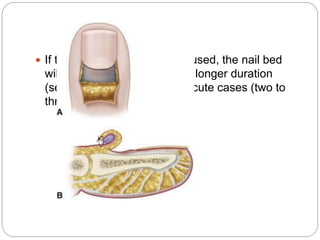
Acute and chronic paronychia are inflammatory conditions of the fingers or toes. Acute paronychia involves a single digit and results from disruption of the nail fold barrier, presenting with rapid onset pain and inflammation. Treatment depends on severity but may include warm soaks, topical antibiotics, and opening any abscesses. Chronic paronychia involves multiple digits and results from irritant dermatitis. Treatment focuses on removing irritants and controlling inflammation with topical steroids or calcineurin inhibitors. Restoring the natural protective barrier can take weeks to months.