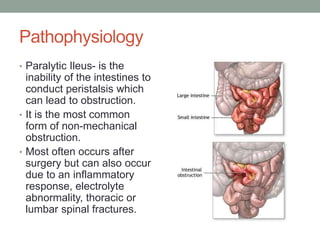
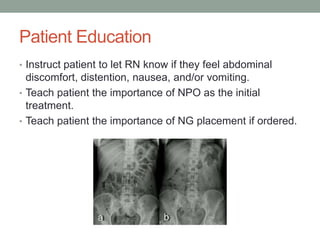
Paralytic ileus is the inability of the intestines to conduct peristalsis, which can lead to obstruction. It most often occurs after surgery but can be caused by inflammation, electrolyte abnormalities, or spinal fractures. Symptoms include colicky abdominal pain, nausea, vomiting, abdominal distension, and constipation. Diagnostic tests like CT scans and x-rays are used, and treatment focuses on resting the bowel with NPO, IV fluids for hydration, and sometimes NG tube placement. Patient education emphasizes reporting changes in symptoms and the importance of treatment compliance.