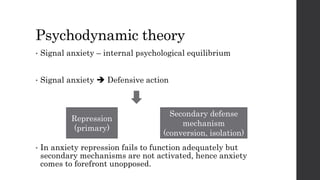
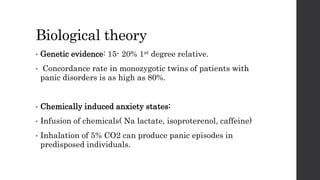
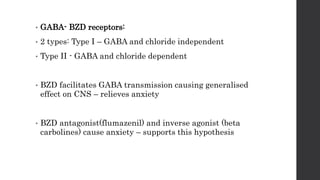
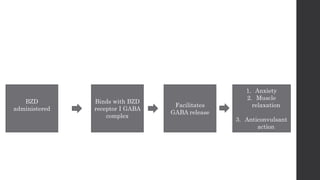
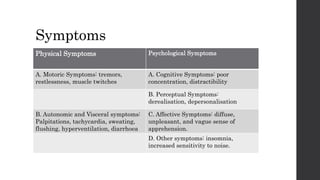
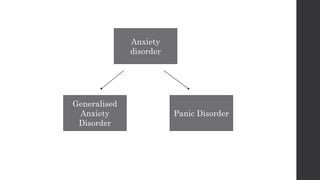
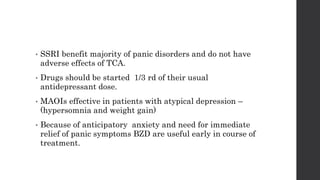
This document discusses panic disorders and their treatment. It defines panic disorder as recurrent, unpredictable panic attacks involving physical symptoms like palpitations, sweating, and fear of losing control. Panic disorder often co-exists with agoraphobia, an anxiety disorder characterized by a marked fear of public places. The document outlines biological, psychological, and cognitive behavioral theories for the causes of panic disorders. Treatment involves both pharmacological options like SSRIs and benzodiazepines as well as non-pharmacological cognitive and exposure therapies.