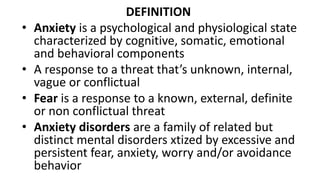
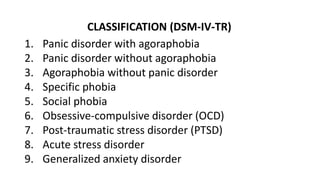
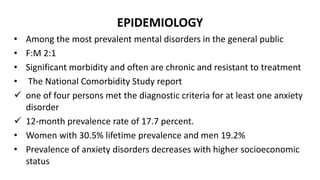
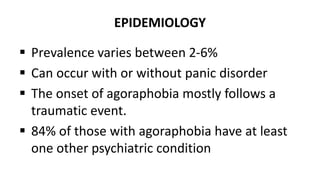
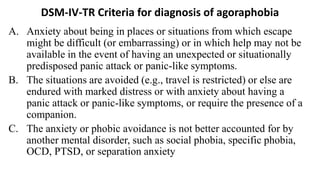
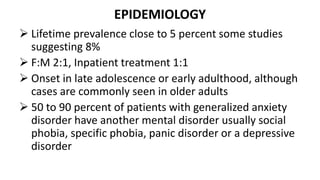
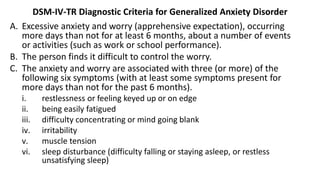
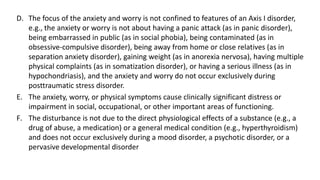
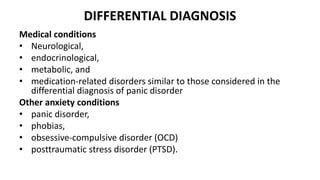
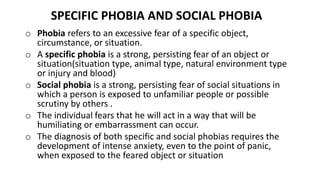
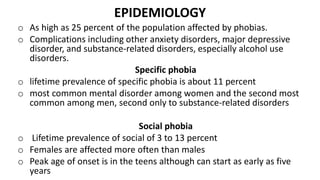
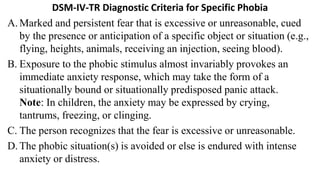
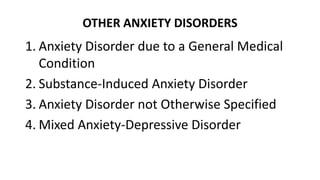
Anxiety disorders are a family of mental disorders characterized by excessive and persistent fear, anxiety, worry and avoidance behaviors. They include panic disorder, agoraphobia, specific phobia, social anxiety disorder, generalized anxiety disorder and obsessive compulsive disorder. Anxiety disorders are highly prevalent, affecting around 1 in 4 people at some point in their lives. They are more common in women and often have an early age of onset. Biological, genetic, psychological and environmental factors all contribute to the development of anxiety disorders.