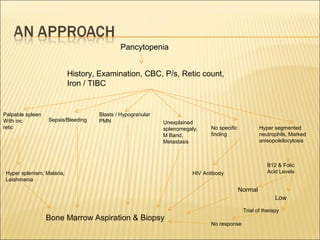
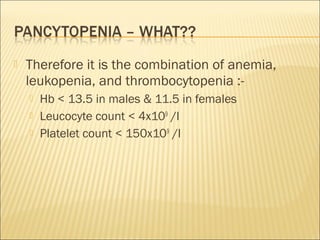
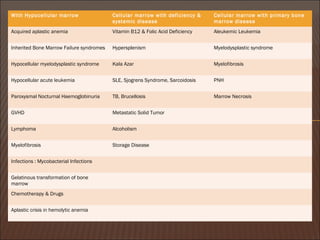
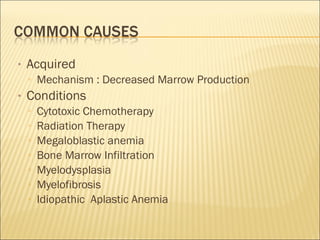
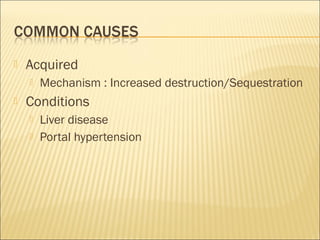
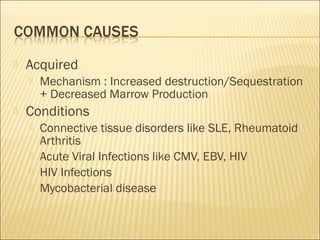
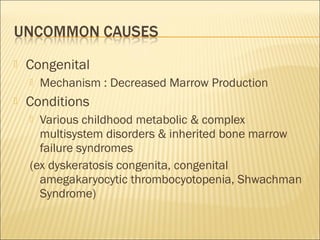
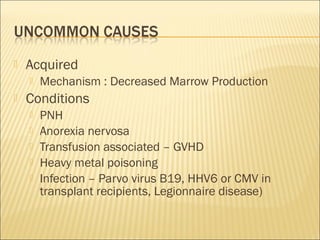
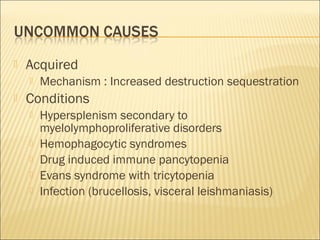
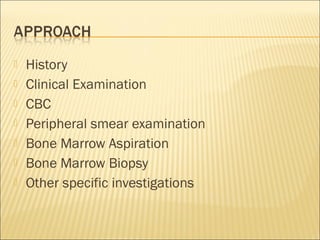
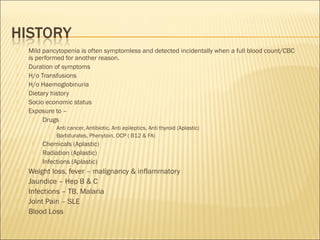
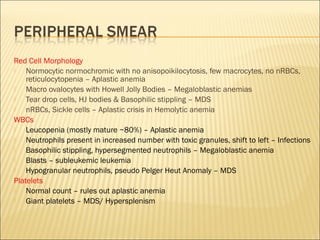
Pancytopenia is a reduction in red blood cells, white blood cells, and platelets. The document outlines an approach to evaluating a case of pancytopenia, including considering decreased bone marrow production, increased cell destruction, a thorough history and physical exam, and diagnostic tests like complete blood count, peripheral smear, and bone marrow aspiration and biopsy to determine the underlying cause. The causes of pancytopenia are grouped based on mechanism and include conditions like aplastic anemia, megaloblastic anemia, myelodysplastic syndrome, liver disease, and others.
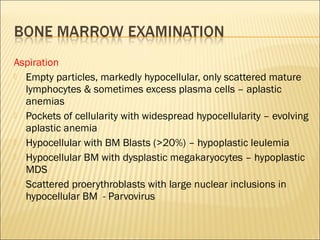
![• Examination of bone marrow is almost always indicated in cases of
pancytopenia unless the cause is otherwise apparent (e.g., established liver
disease with portal hypertension).
• The bone marrow exam consists of both an aspirate and a trephine biopsy,
• The differential diagnosis of pancytopenia may be broadly classified based
on the
▫ bone marrow cellularity (reduced cellularity indicates decreased production of blood cells,
▫ whereas normal/increased cellularity indicates ineffective production or increased
destruction or sequestration of blood cells).
• Specifically, bone marrow aspirate permits examination of:
• Cytology (megaloblastic change, dysplastic changes, abnormal cell
infiltrates, hemophagocytosis, and infection [e.g., Leishman-Donovan
bodies])
• Immunophenotyping (acute and chronic leukemias, lymphoproliferative
disorders)
• Cytogenetics (myelodysplasia, acute and chronic leukemias,
lymphoproliferative disorders).](https://image.slidesharecdn.com/pancytopeniavishu-140422202134-phpapp01/85/Pancytopenia-Approach-23-320.jpg)