Pancreatitis is an inflammation of the pancreas that can be acute or chronic. The most common causes are biliary issues, alcohol use, and idiopathic factors. Patients present with epigastric pain radiating to the back that is worse with eating and improved by leaning forward. Diagnosis involves pancreatic enzyme levels and imaging. Treatment is supportive with IV fluids, analgesics, monitoring for complications, and treating underlying causes. Complications can include necrosis, infection, pseudocysts, and systemic impacts. Prognosis depends on the presence of organ failure.
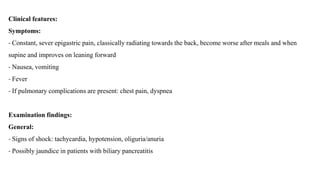
![Laboratory tests:
- CBC (↑ WBC and Hematocrit)
- Renal panel
- Liver panel (↑ liver enzymes and bilirubin in biliary pancreatitis)
- Pancreatic enzymes [Amylase and Lipase (more sensitive and specific)] (often normal in chronic pancreatitis).
Note: not necessarily correlate with severity of inflammation
- ESR, CRP and LDH (severity marker)
- Triglyceride
- Calcium level](https://image.slidesharecdn.com/pancreatitis-221227193636-52c480b7/85/pancreatitis-8-320.jpg)
![Treatment of Infected necrotizing pancreatitis:
1- Broad-spectrum empiric antibiotics with good tissue penetration (e.g., carbapenems) for 4 weeks.
2- Drainage of infected material if there is clinical deterioration or persistence of symptoms despite antibiotic
therapy:
- Operative pancreatic debridement (necrosectomy) should ideally be performed at least 2–4 weeks after initial
presentation. [14]
- Minimally invasive procedures (e.g., image-guided percutaneous drainage) can be performed in the first 2
weeks in seriously ill patients.](https://image.slidesharecdn.com/pancreatitis-221227193636-52c480b7/85/pancreatitis-25-320.jpg)