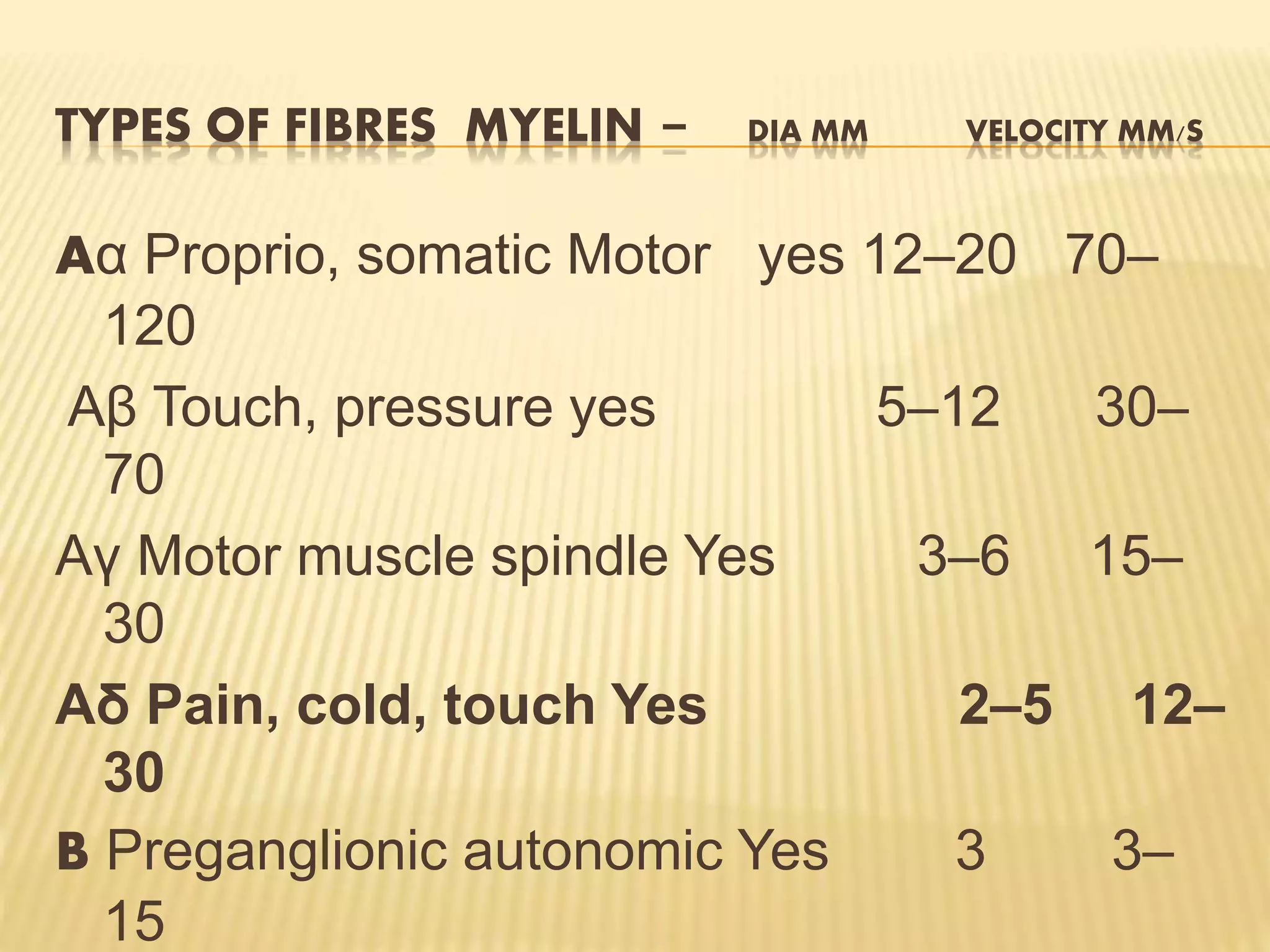
Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage. It is classified in several ways including by type (nociceptive, neuropathic, psychogenic), duration (acute, chronic), and location. Theories of pain transmission include the specificity, pattern, and gate control theories. Pain signals travel along A-delta and C fibers to the spinal cord and then ascend to the brain via the spinothalamic tract. Descending pathways from the brainstem modulate pain transmission through the release of neurotransmitters like serotonin and norepinephrine.