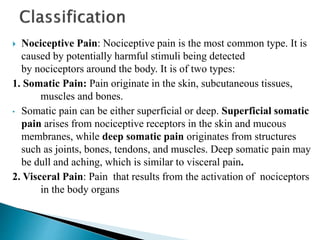
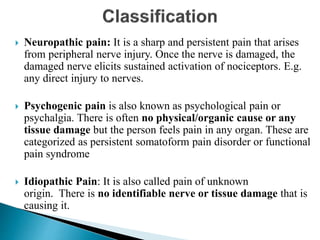
This document provides an overview of a lecture on pain. It begins with the lecturer's name and credentials. The objectives of the lecture are then outlined, which include defining pain, differentiating between acute and chronic pain, and explaining pain management approaches. The document proceeds to discuss topics like nociceptors, the somatosensory pathway, endogenous pain mechanisms, and classifications of pain. Pathophysiological processes underlying pain are explored. Non-pharmacological pain management strategies like TENS, heat/cold therapy are also summarized.




























![Transcutaneous electrical nerve stimulation acts by the
concept of Gate Control Theory.
Selectively stimulate the A beta fibers [mechanoreceptive
fibers (touch, vibration e.t.c.)] by titrating the amplitude
of electrical current delivered across the surface of the
skin.
This would prevent signals from nociceptive fibers from
reaching higher centers of the brain, thus reducing pain.](https://image.slidesharecdn.com/pain-230514095206-156b1d72/85/PAIN-ppt-32-320.jpg)



