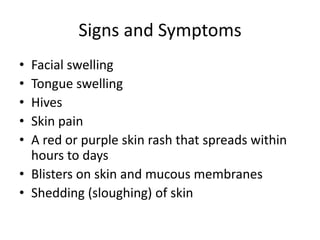
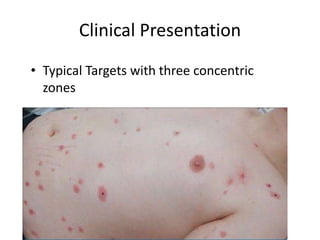
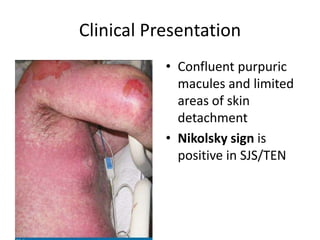
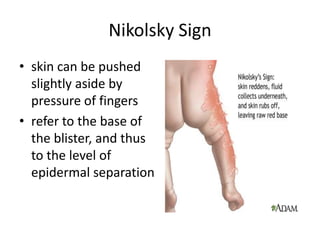
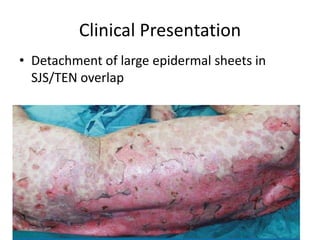
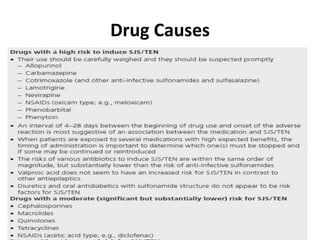
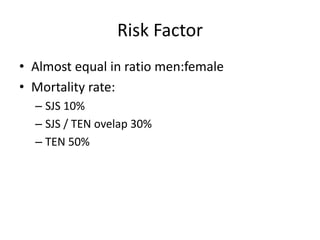
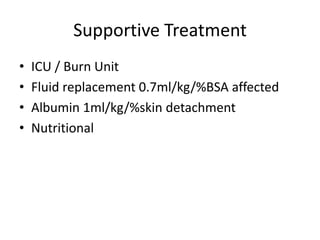
SJS and TEN are life-threatening mucocutaneous diseases within the spectrum of severe cutaneous adverse reactions (SCAR) that can be caused by drugs, infections, or unknown factors. They involve epidermal necrosis and sloughing of the skin and mucosal surfaces. SJS usually presents as less severe than TEN. While no treatment can halt skin detachment progression, supportive care including fluid replacement, nutrition, analgesics, and antibiotics when needed is crucial, though mortality increases with severity and underlying patient conditions.