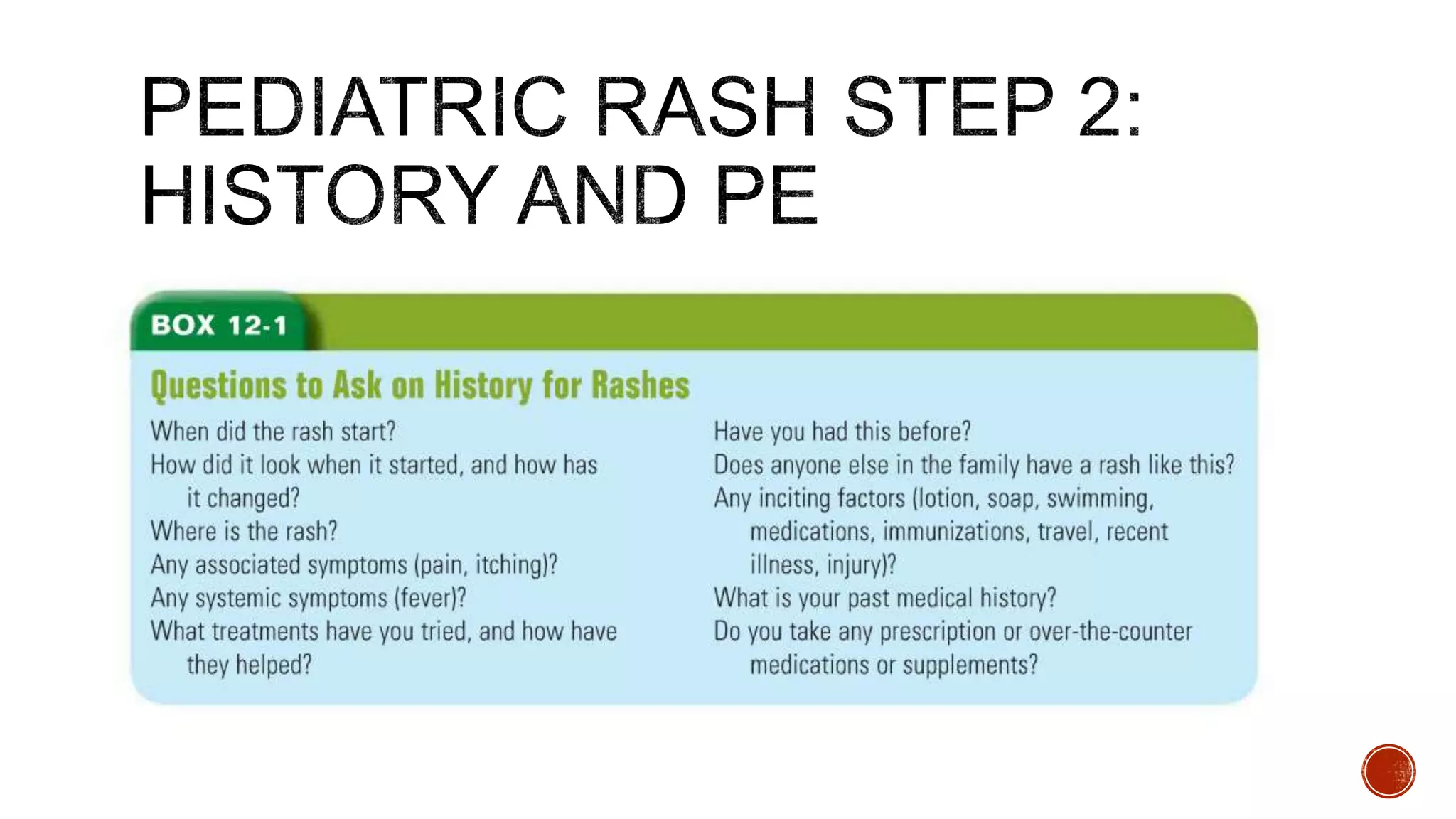
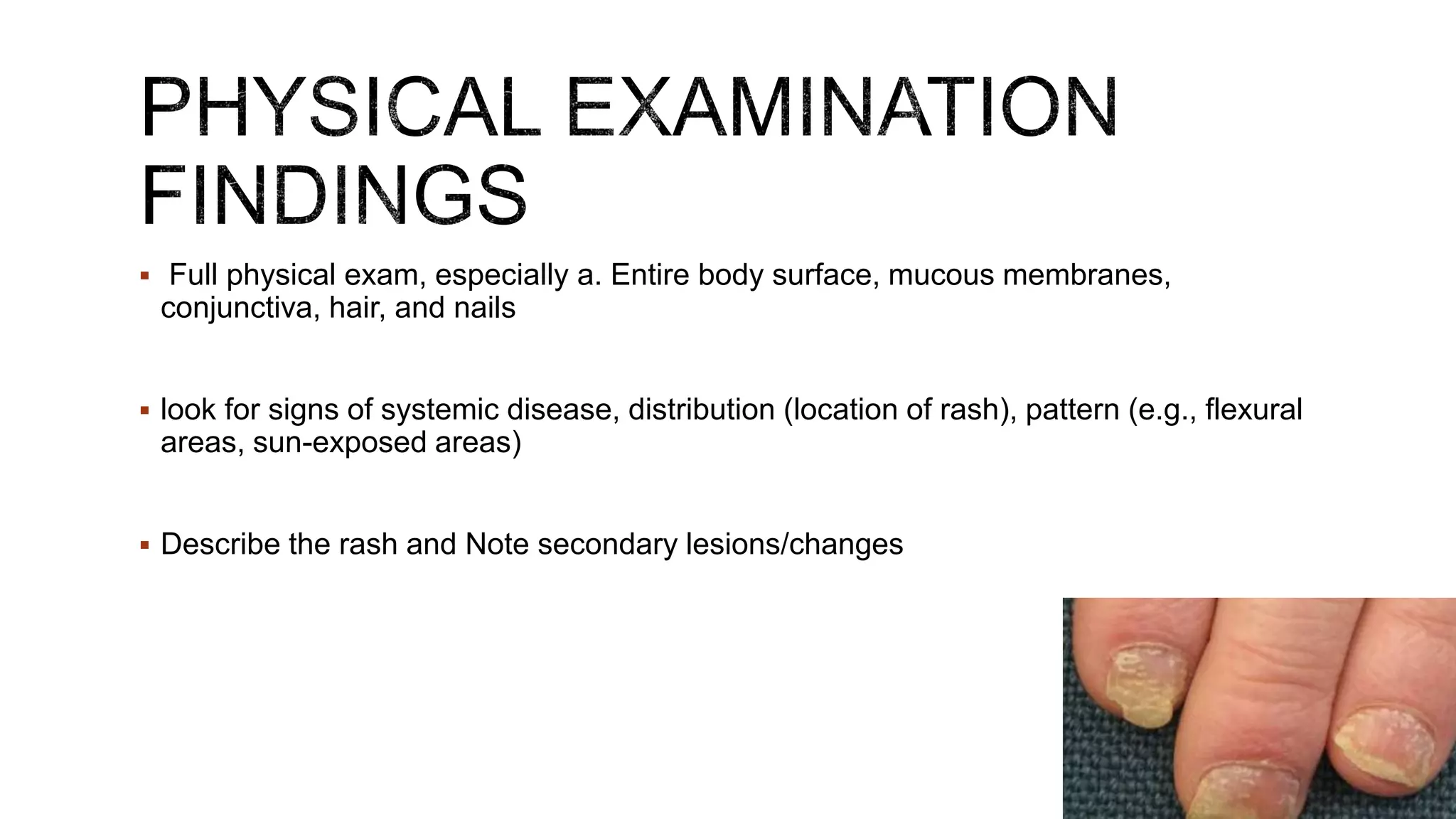
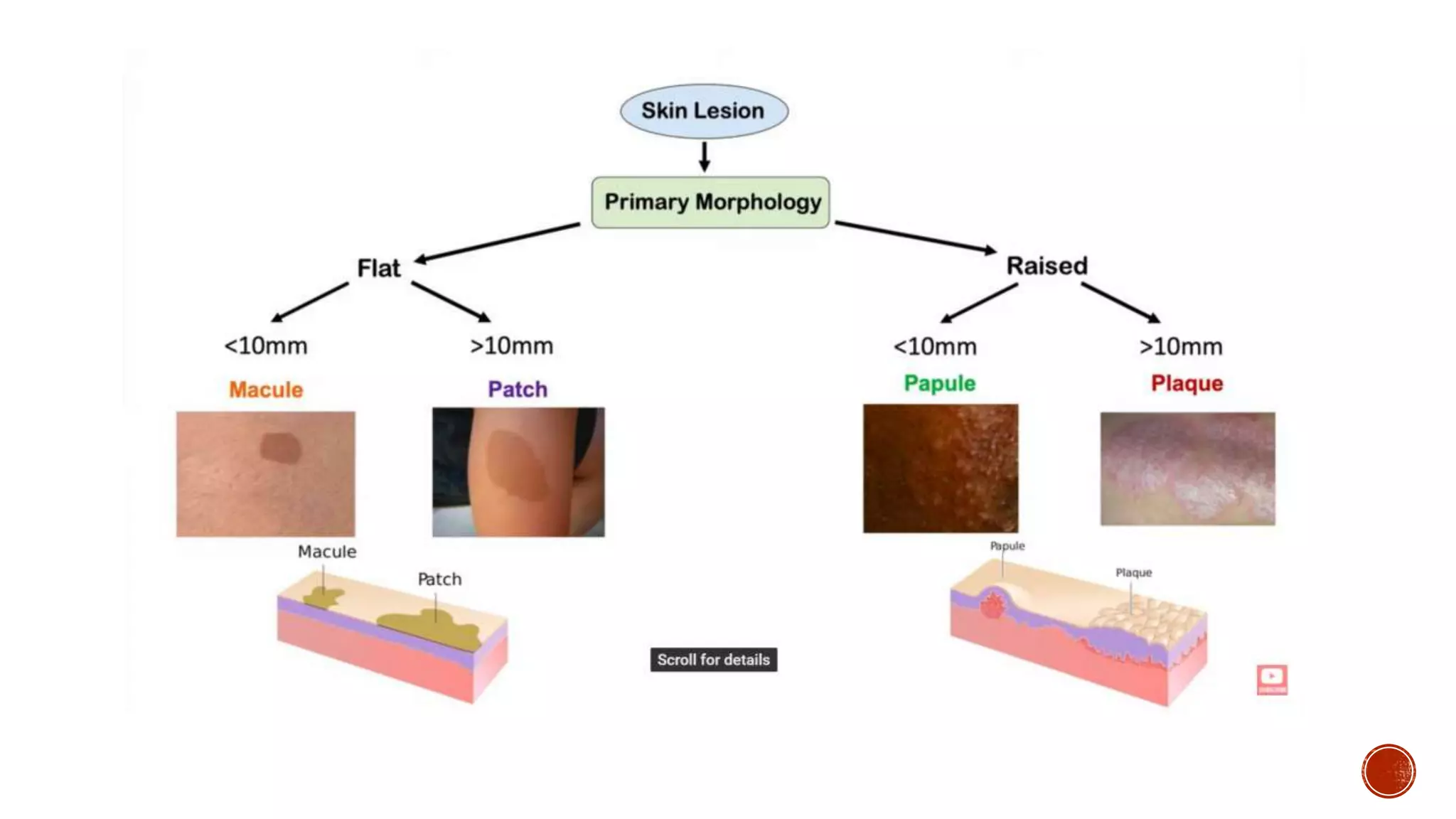
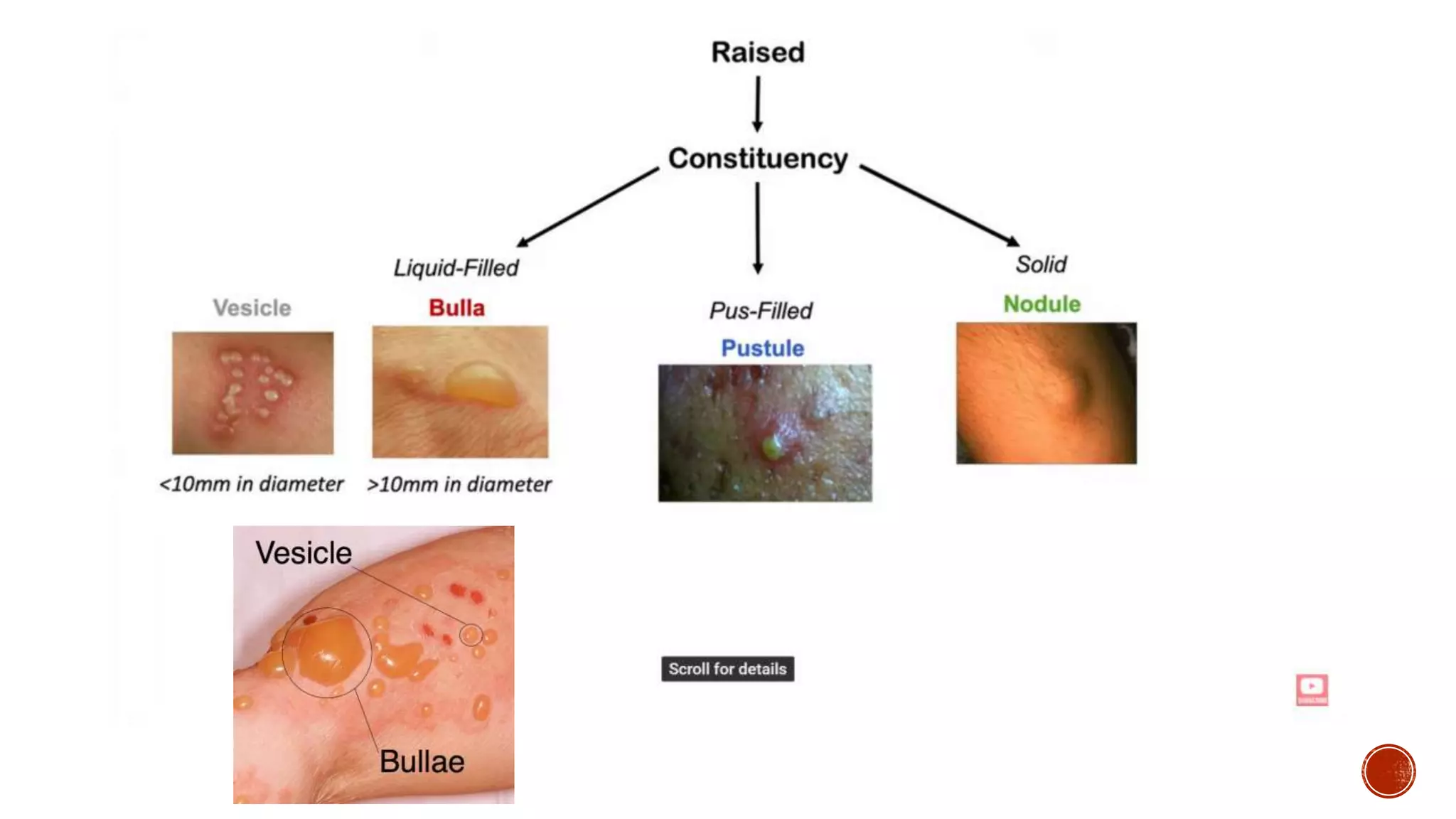
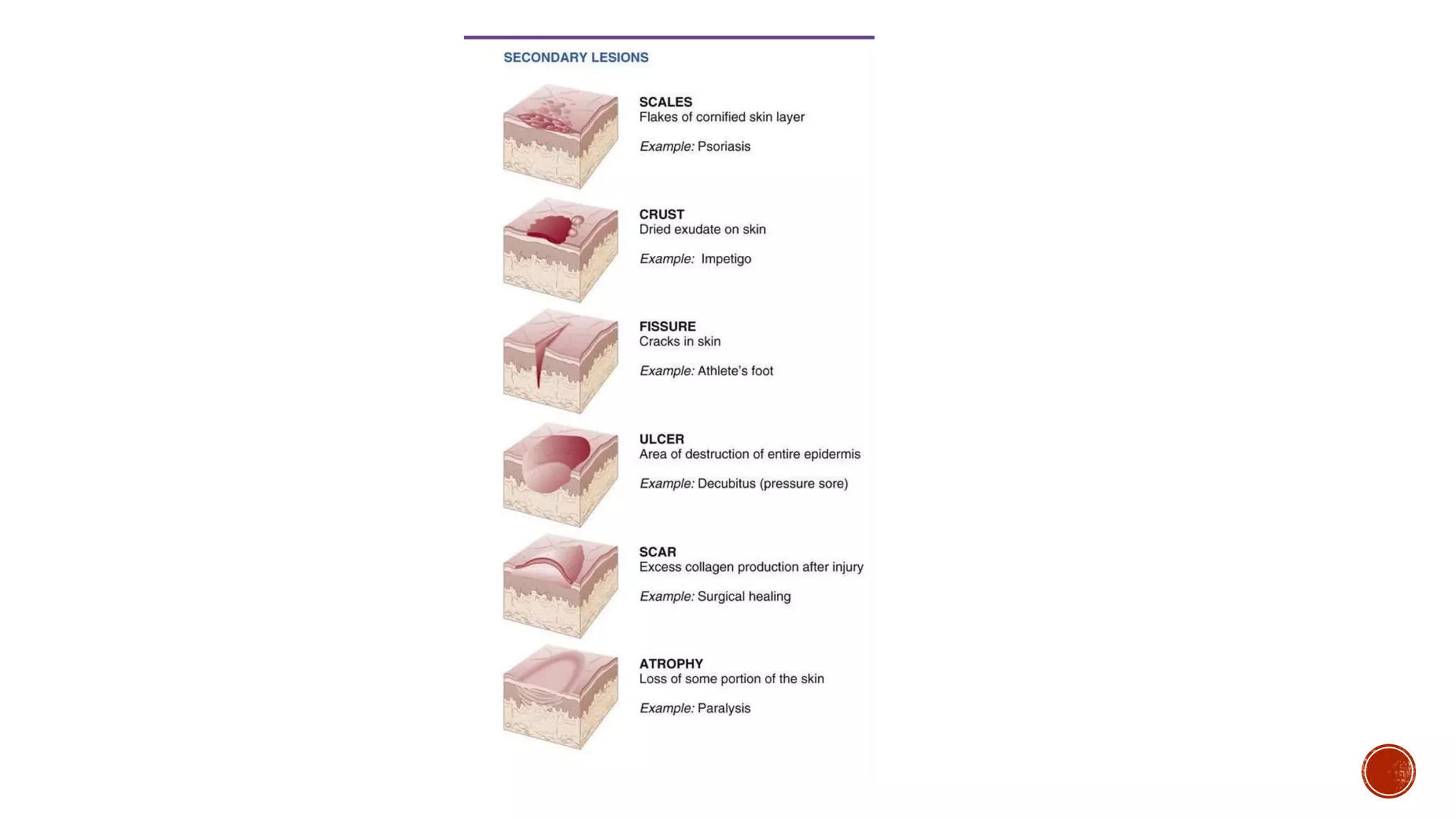
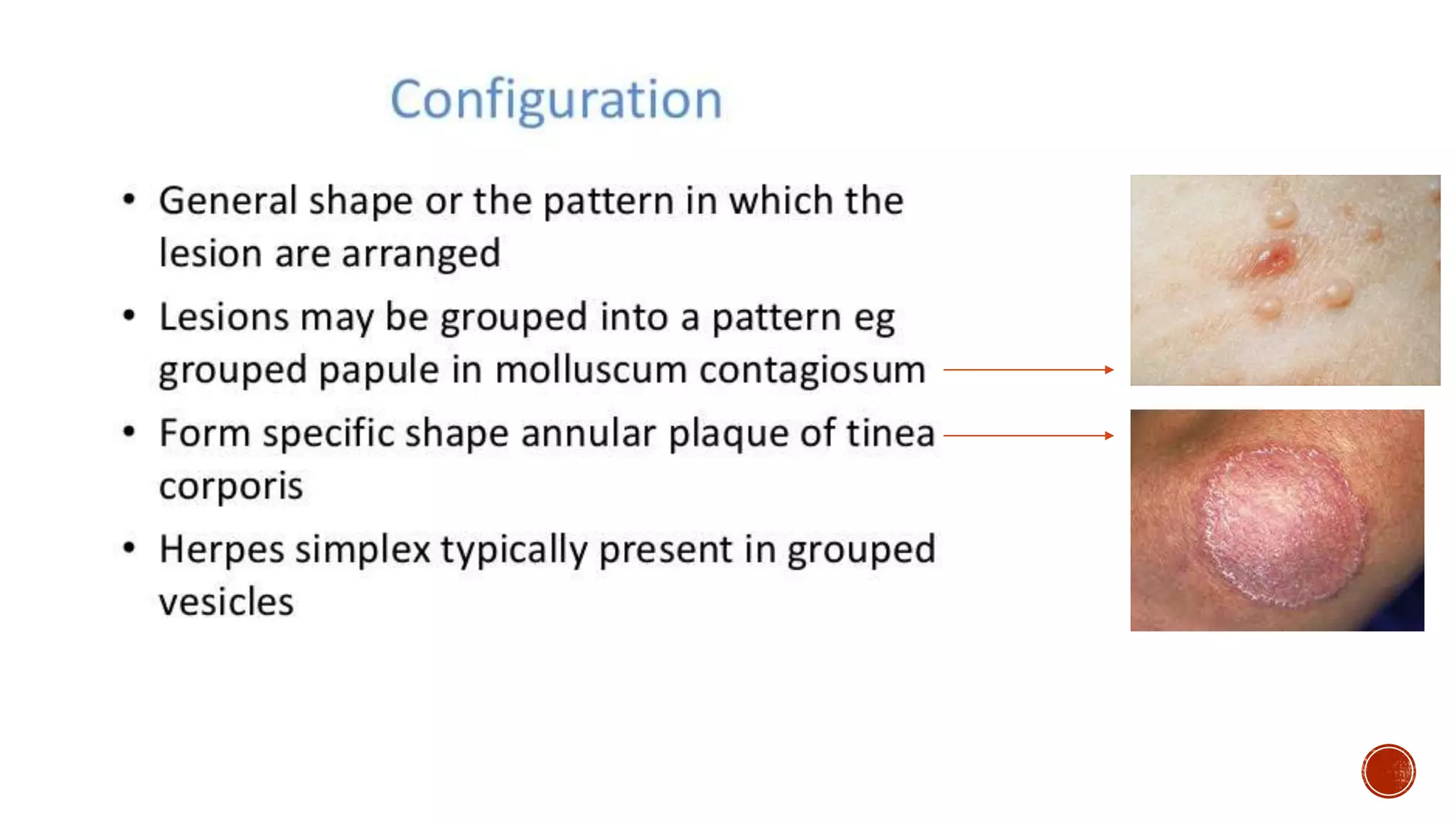
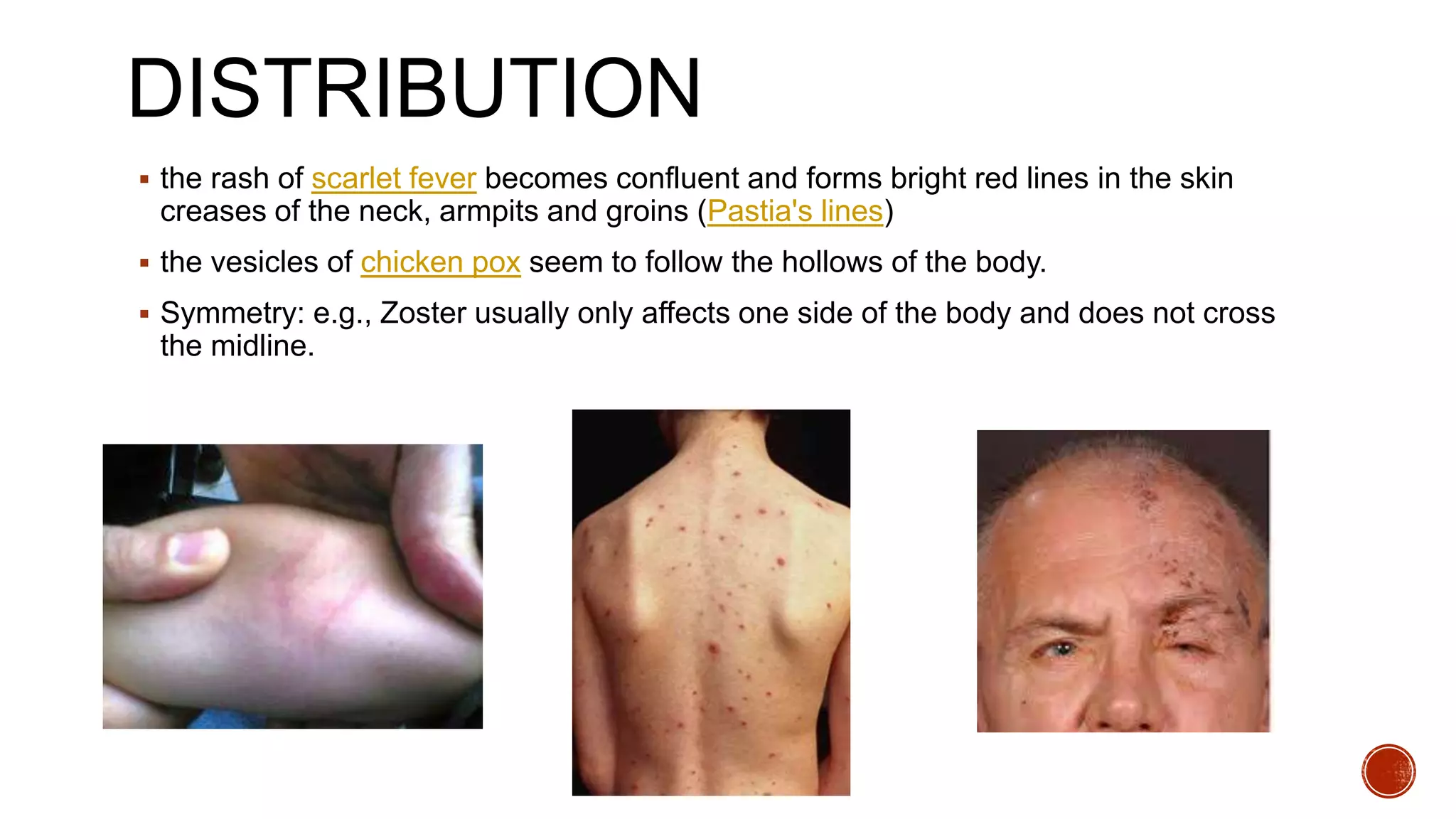
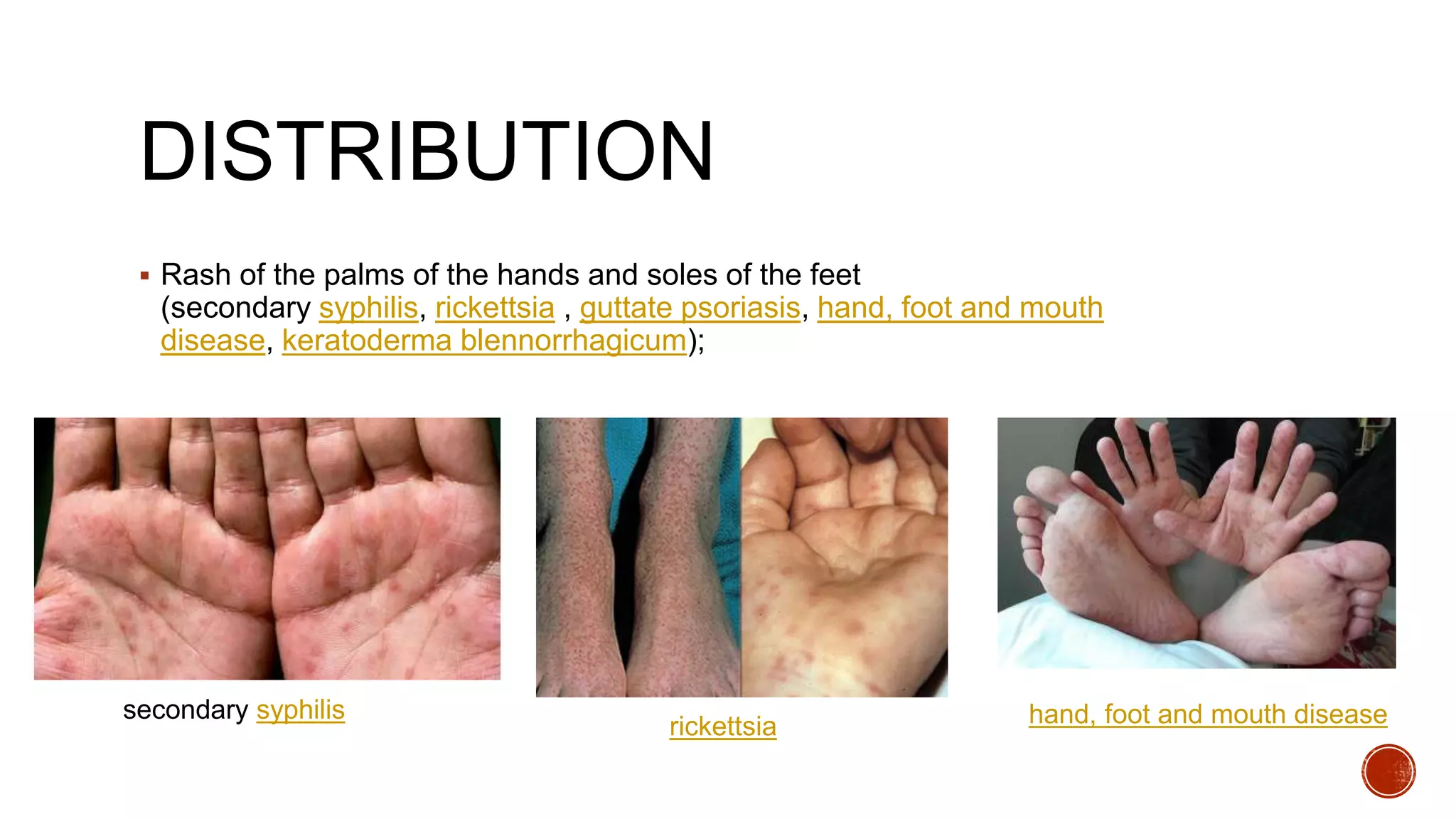
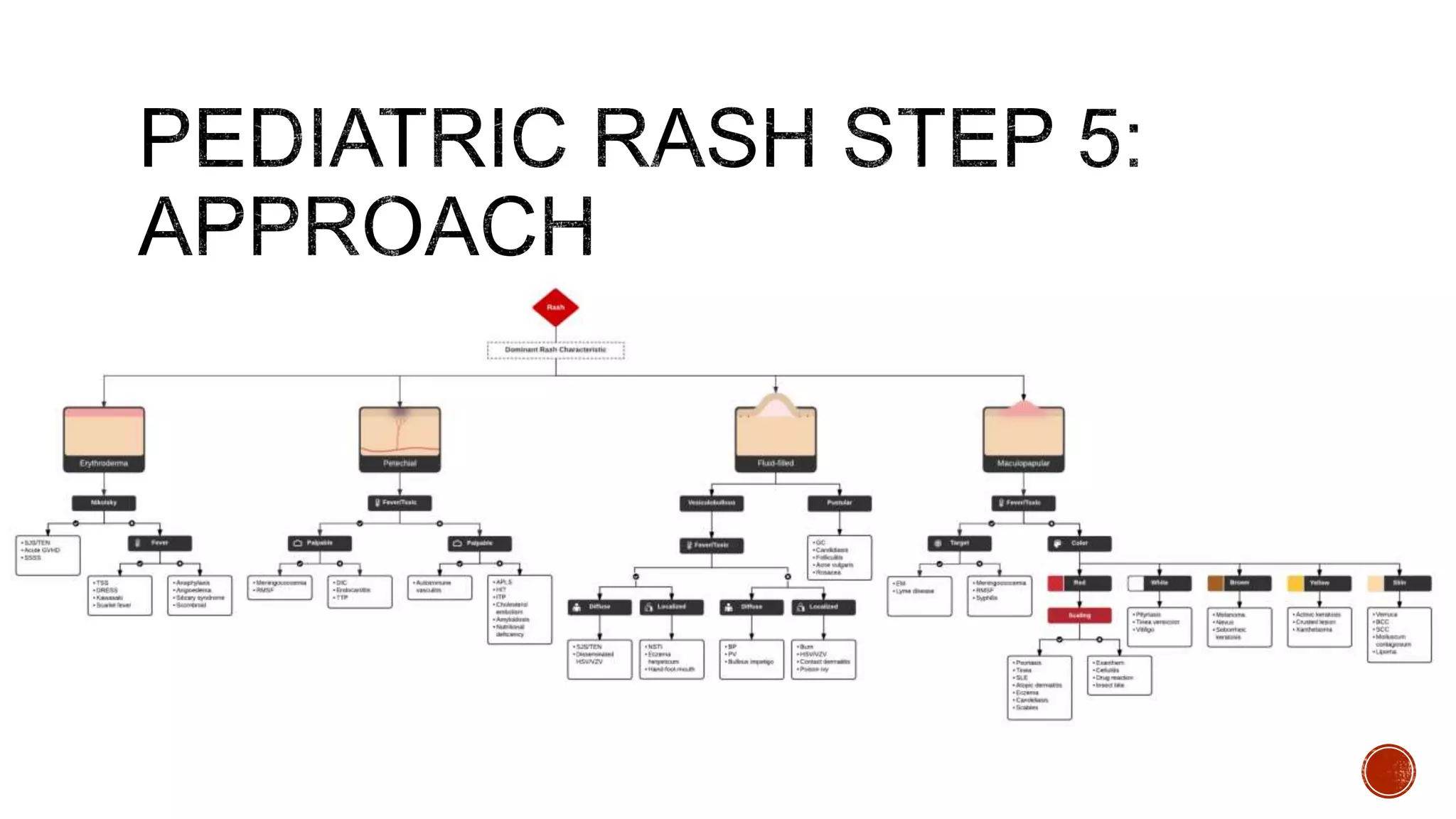
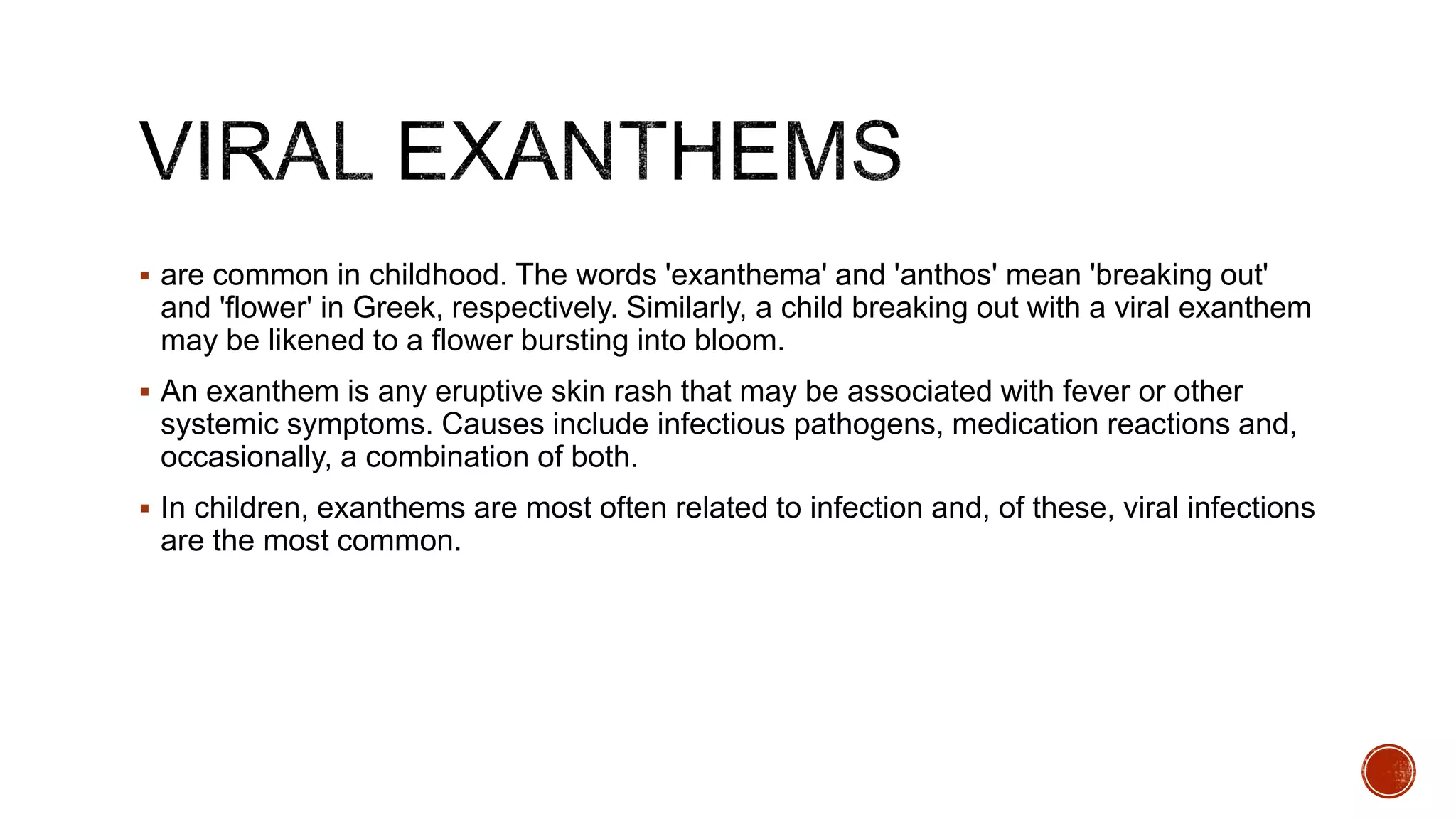
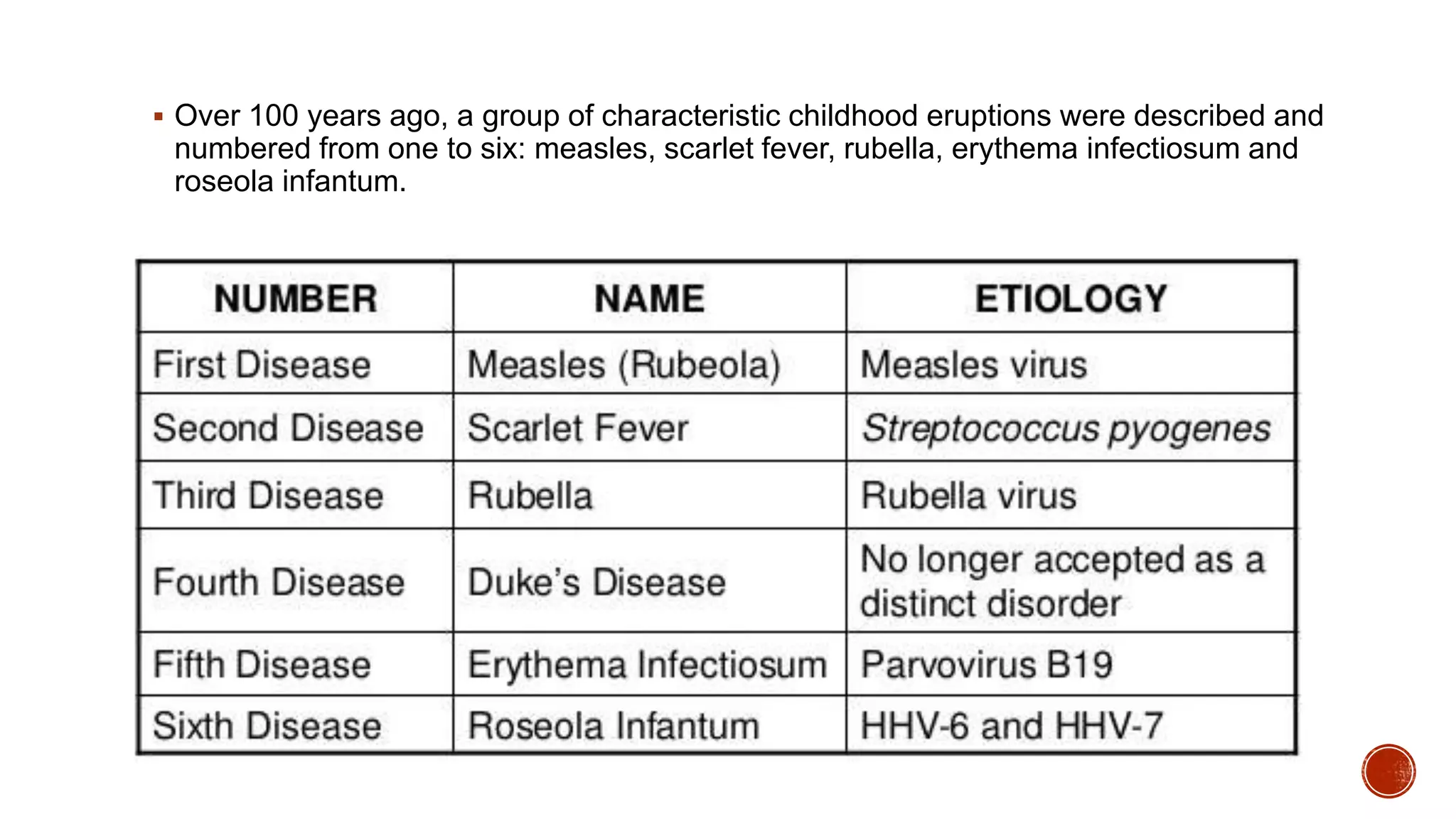
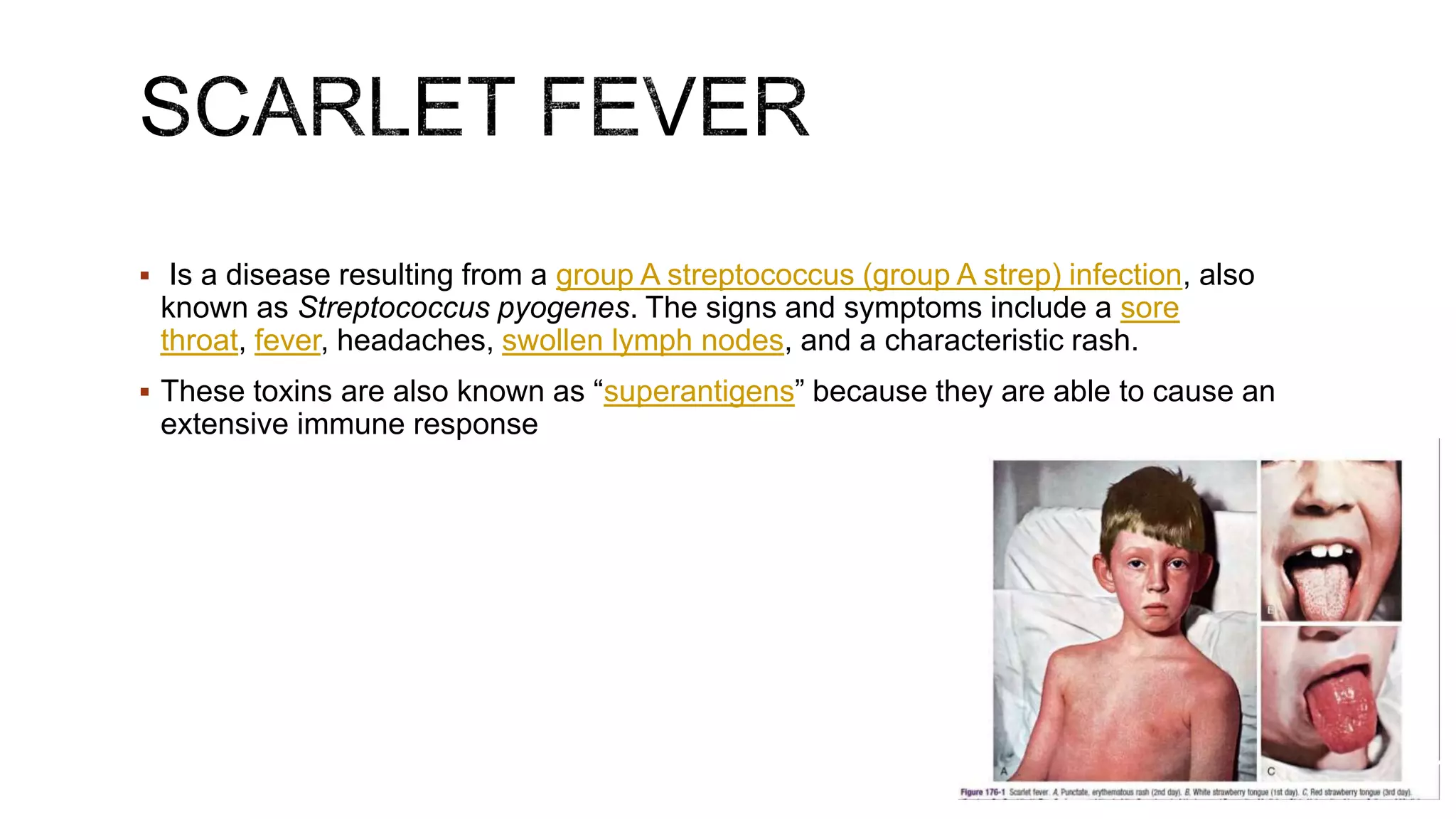
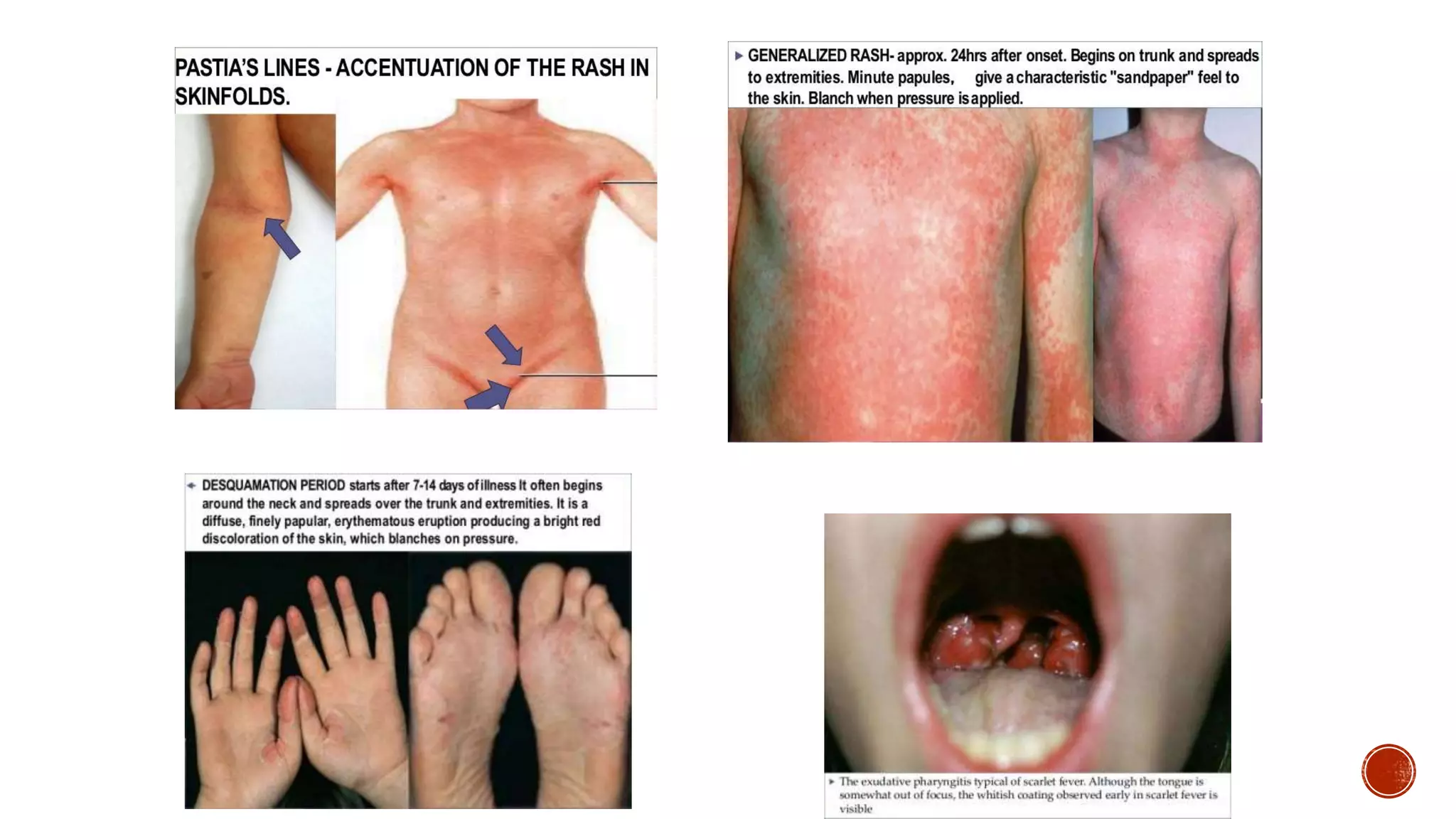
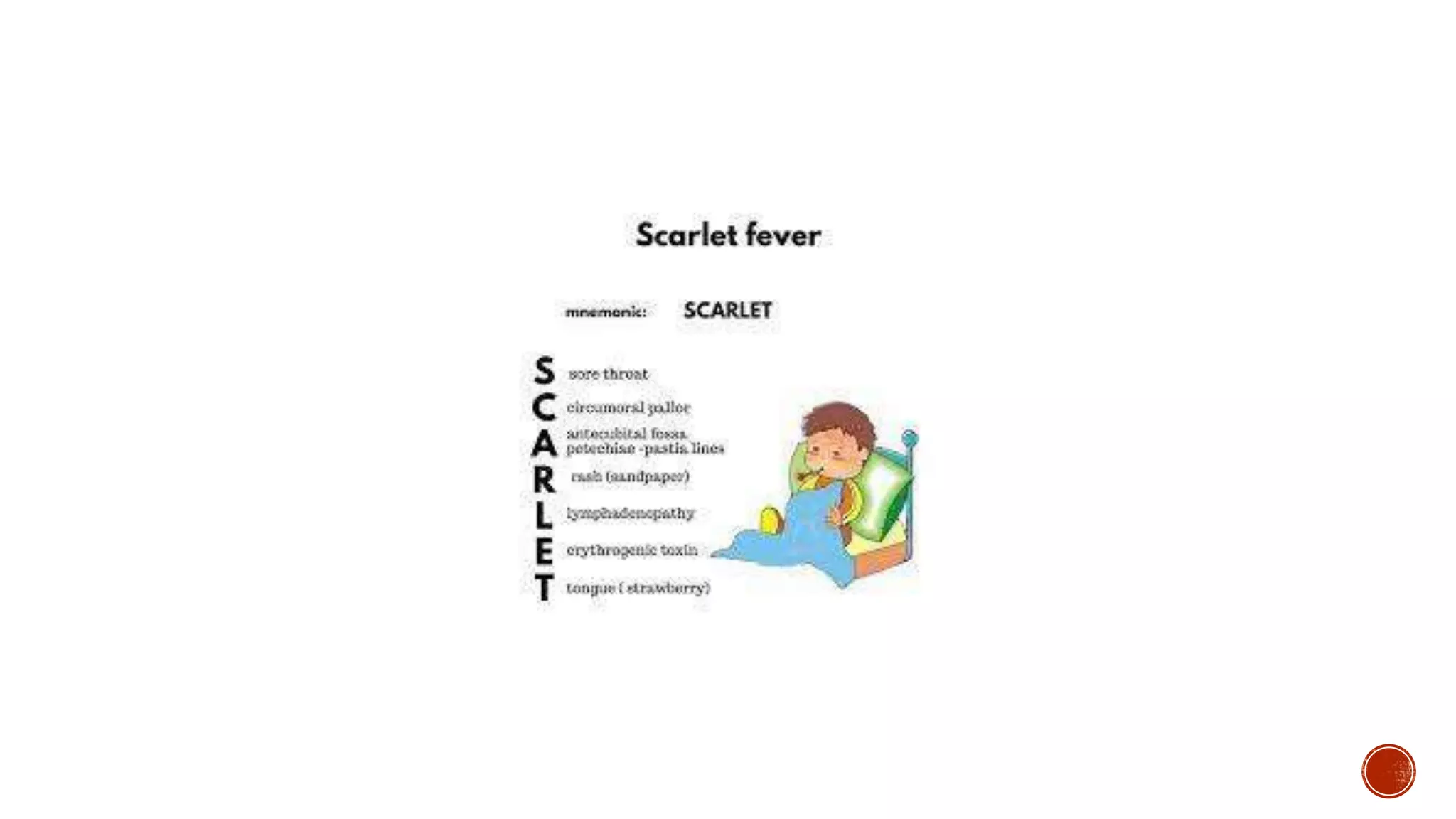
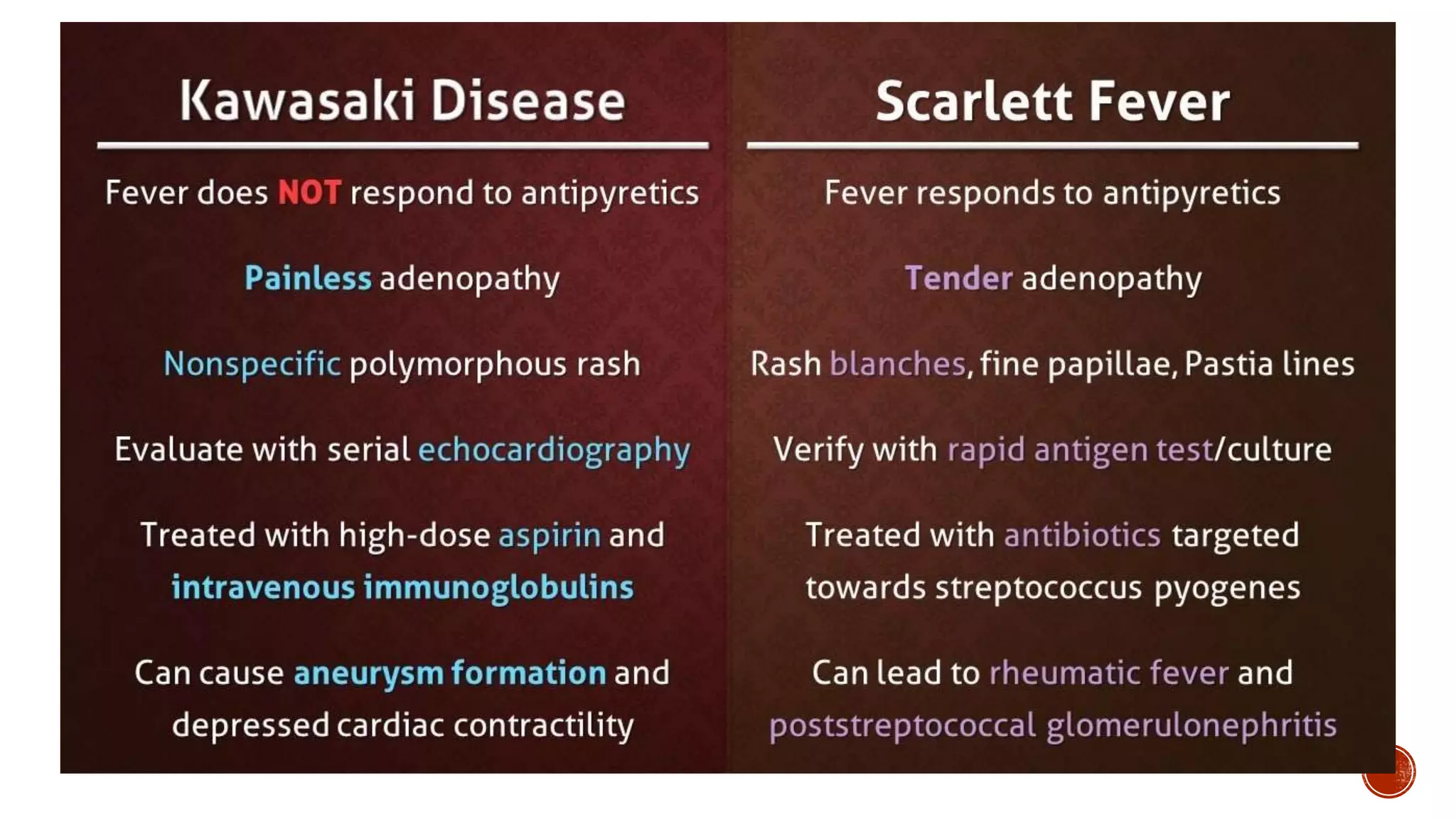
The document provides a comprehensive overview of rashes, detailing their classifications, potential causes, and relevant patient evaluation techniques in clinical settings. It emphasizes the importance of thorough history taking and physical examination to identify underlying conditions while being aware of red flags that may indicate serious pathology. The text also includes specific considerations for children's rashes and common infectious conditions that present with cutaneous manifestations.


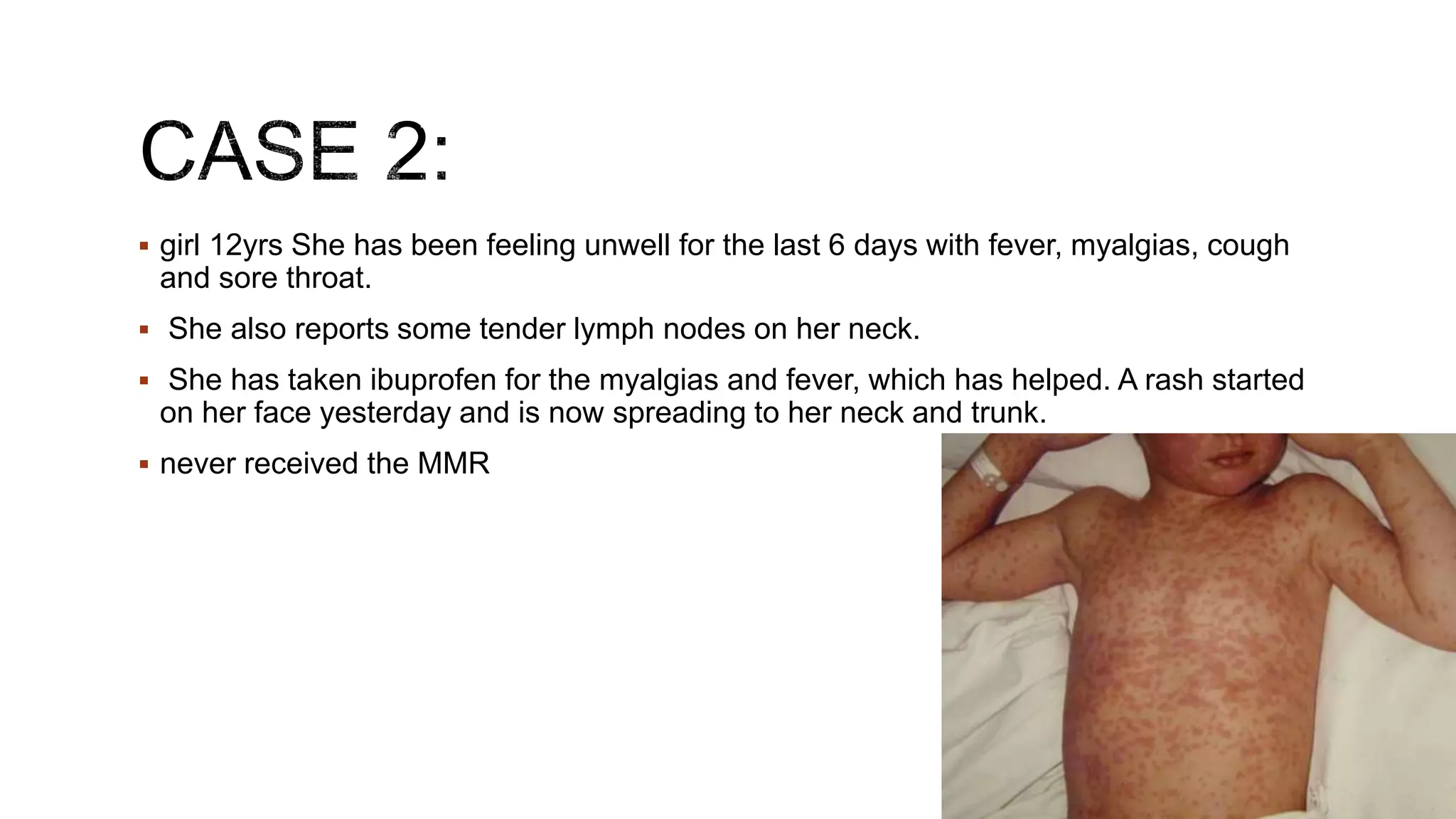
![SICK
In the ER
Sick?
Treat aggressively!
The skin findings may help clue you in to the source of the sickness, but don’t let pontification
of the unusual rash delay your rapid administration of necessary care!
Historical and physical “red flags” in a patient with an unknown rash include:[1]
Severe pain
Very old or young age
Immunosuppressed
New medication
Fever
Toxic appearance
Hypotension
Mucosal lesions](https://image.slidesharecdn.com/skinrash-210724115222/75/Approach-to-Skin-rash-3-2048.jpg)