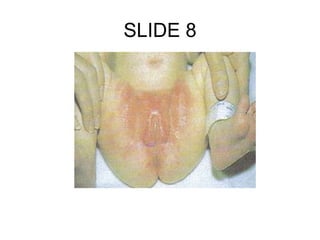
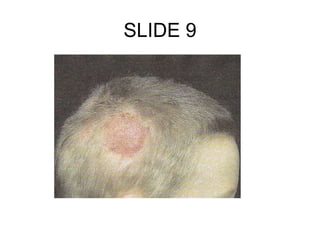
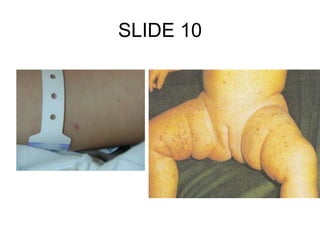
1. The document discusses various pediatric dermatological conditions and rashes seen in children.
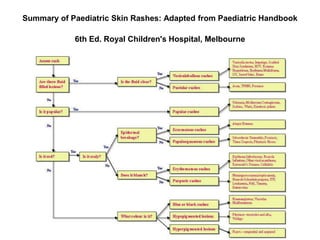
2. It provides terminology used to describe skin lesions and summarizes common pediatric skin rashes.
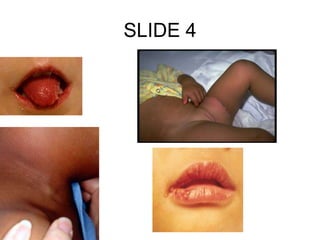
3. The remainder of the document consists of slides that each discuss a different skin condition or rash, naming it, describing features, causes, and typical treatment approaches.