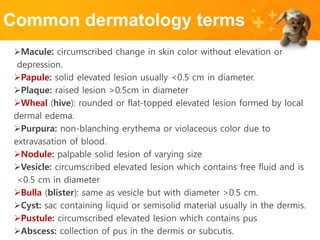
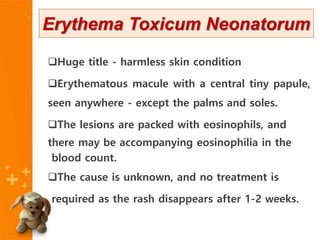
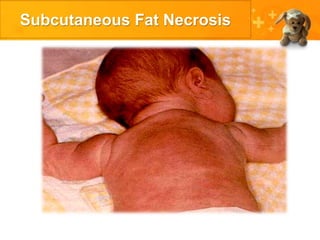
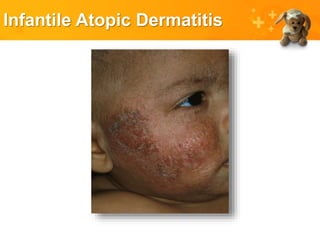
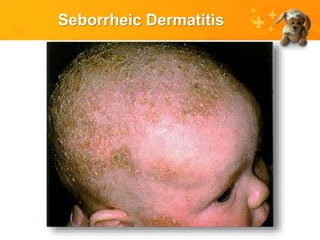
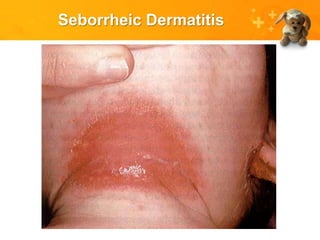
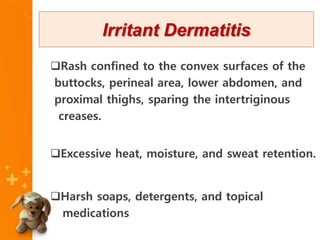
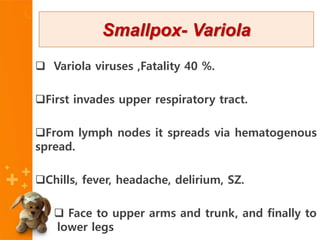
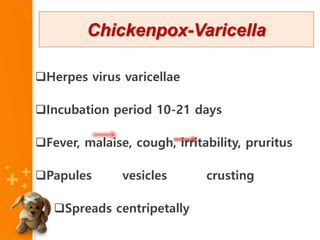
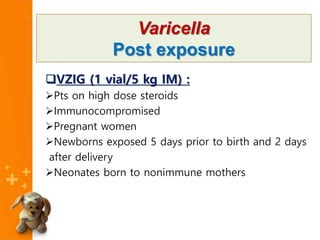
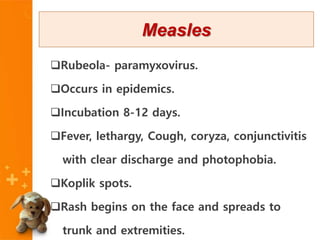
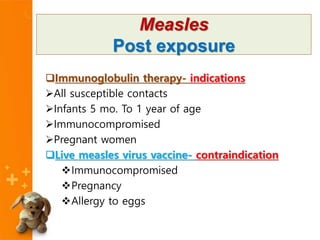
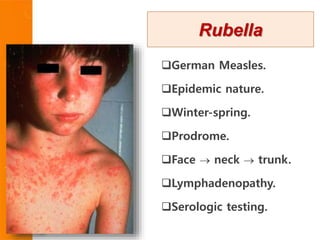
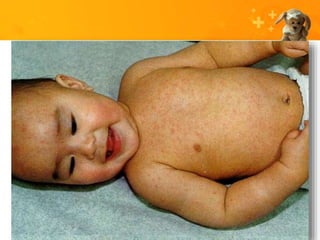
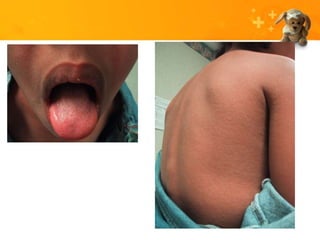
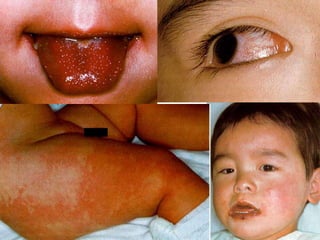
This document defines common dermatology terms like macule, papule, plaque, wheal, and provides descriptions of primary skin lesions including erythema toxicum neonatorum, miliaria, subcutaneous fat necrosis, infantile atopic dermatitis, seborrheic dermatitis, candidal dermatitis, irritant dermatitis and describes various infectious exanthems like measles, rubella, hand-foot-mouth disease, erythema infectiosum, exanthem subitum, infectious mononucleosis, impetigo, scarlet fever, meningococcemia, Rocky Mountain spotted fever, Henoch-Schnlein purpura and Kawasaki