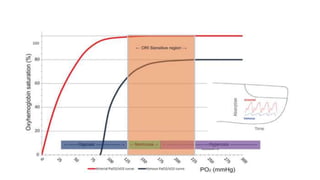
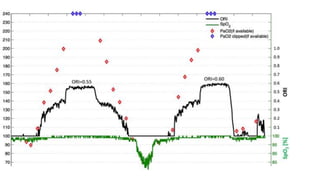
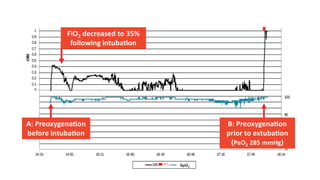
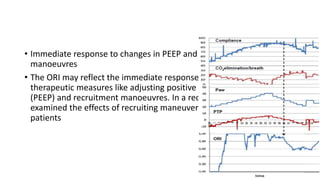
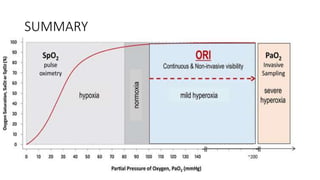
This document discusses the oxygen reserve index (ORI), a new method for continuously monitoring oxygen therapy using multi-wavelength pulse oximetry. The ORI provides information about a patient's oxygenation status beyond what can be determined by pulse oximetry alone. It may help clinicians better titrate supplemental oxygen to prevent hypoxemia and hyperoxemia. Preliminary studies show the ORI can detect impending desaturations earlier than pulse oximetry and correlates with measured oxygen levels. Potential applications of the ORI include optimizing oxygen administration, preoxygenation, and assessing the effects of interventions like changes to PEEP. However, further research is still needed to validate its clinical utility.