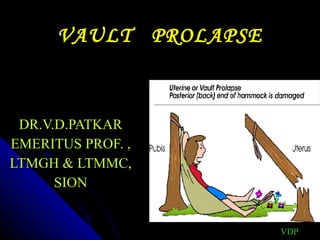
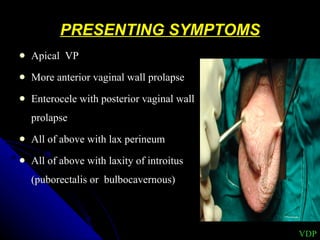
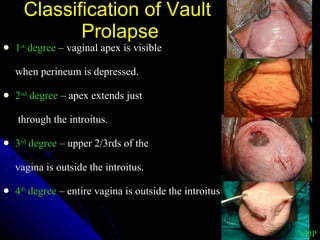
1. Vault prolapse is a distressing complication that can occur after hysterectomy where the top of the vagina descends.
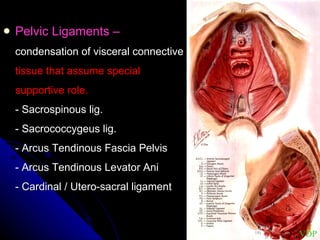
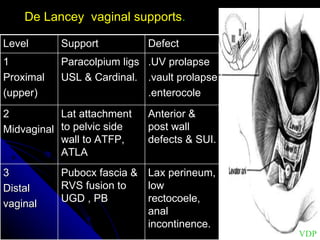
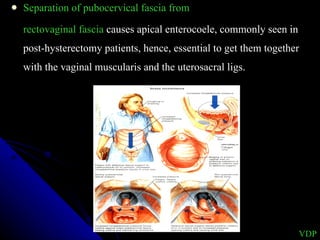
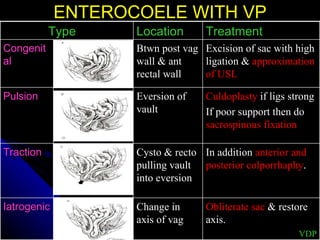
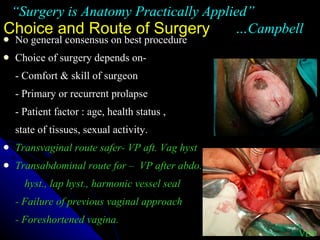
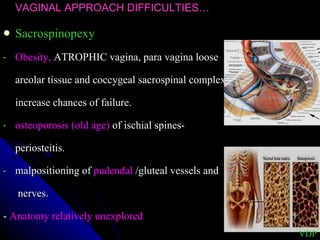
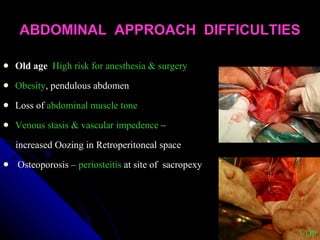
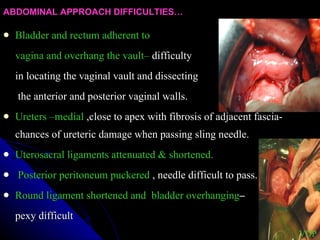
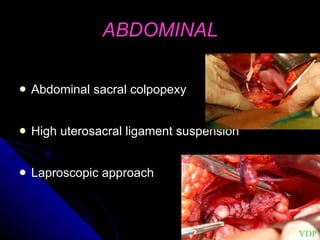
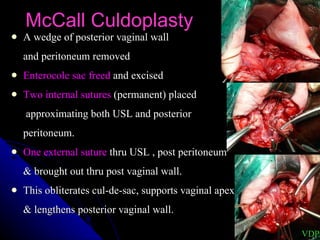
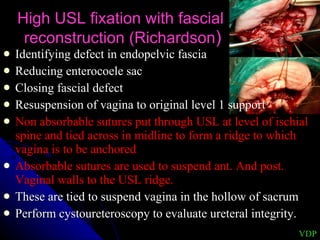
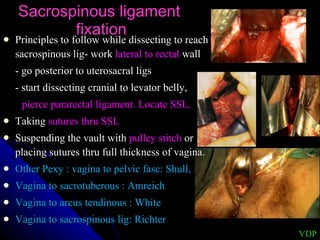
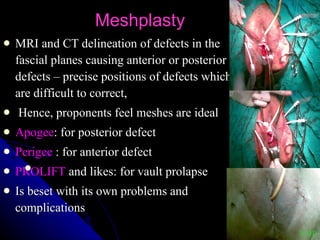
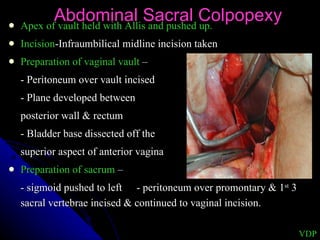
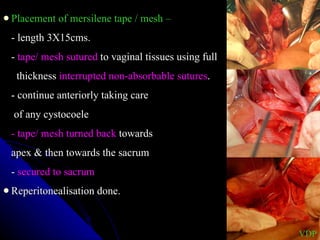
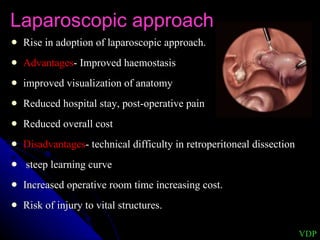
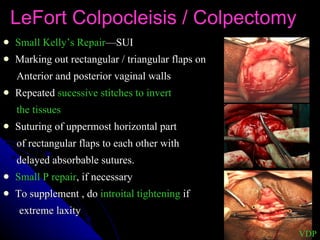
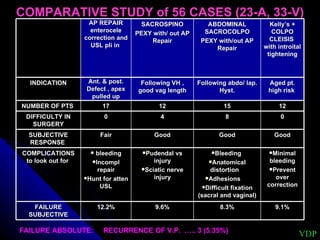
2. There are various surgical options to correct vault prolapse including vaginal approaches like sacrospinous ligament fixation or abdominal approaches like abdominal sacral colpopexy.
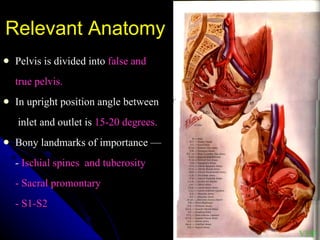
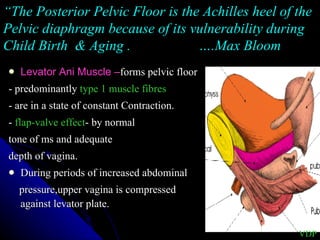
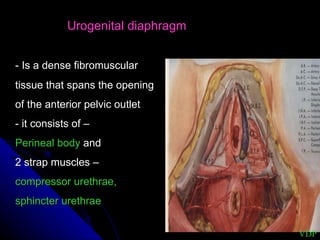
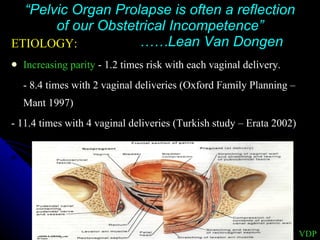
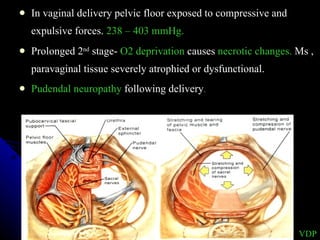
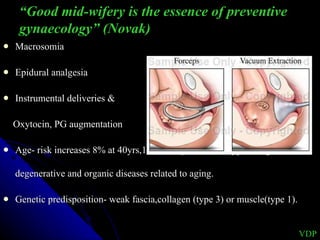
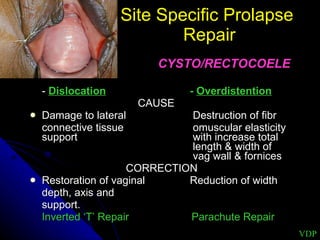
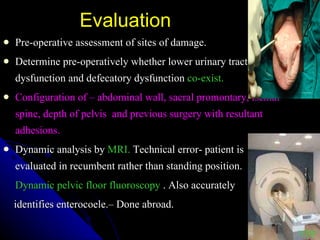
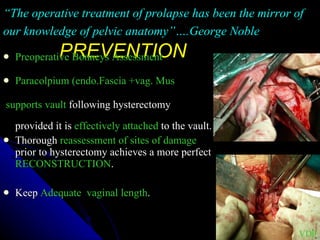
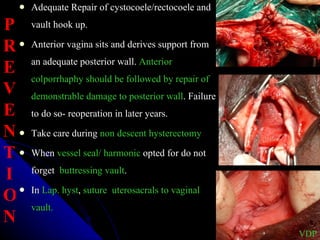
3. Factors like parity, age, and previous pelvic floor damage affect the risk of vault prolapse. Thorough understanding of pelvic anatomy and meticulous repair of cystoceles and rectoceles can help prevent future prolapse.