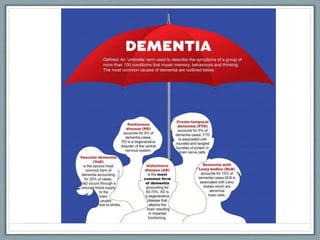
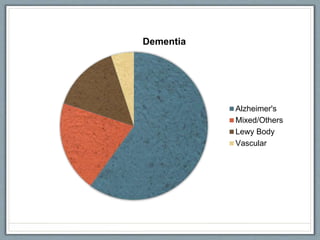
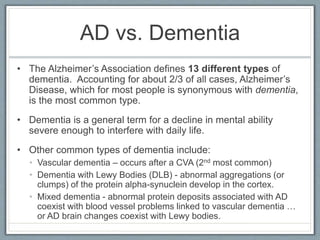
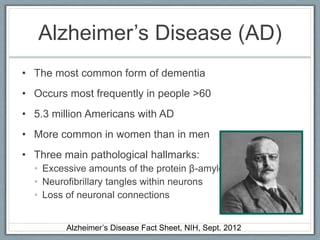
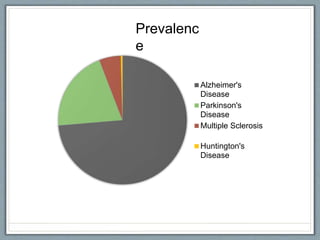
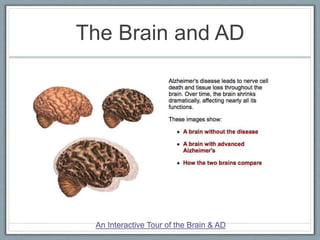
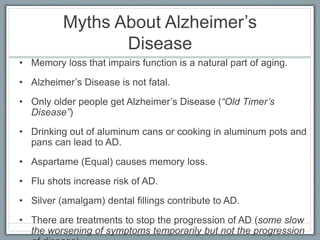
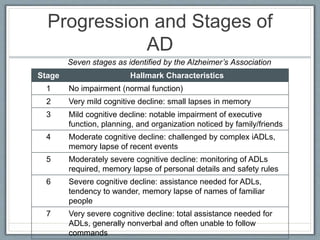
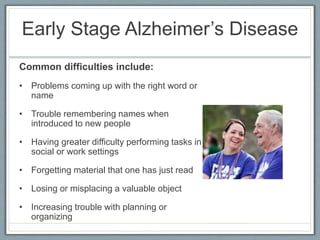
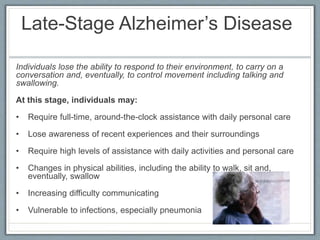
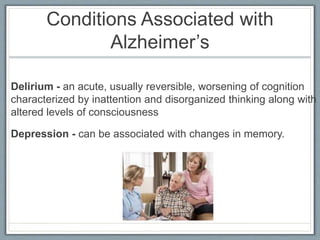
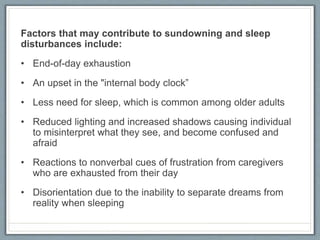
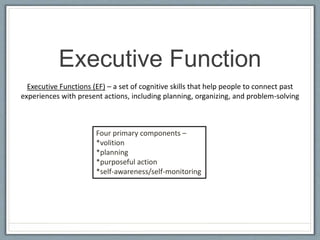
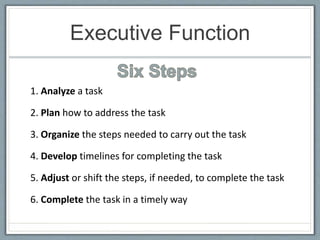
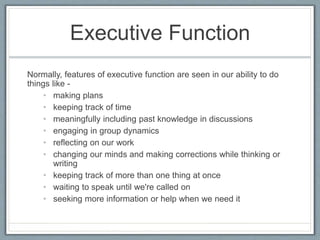
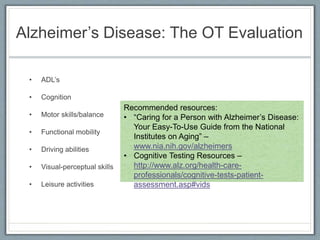
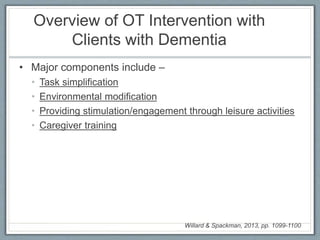
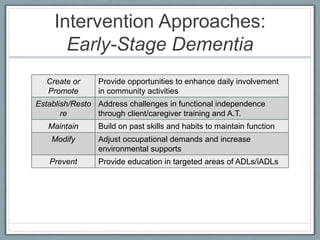
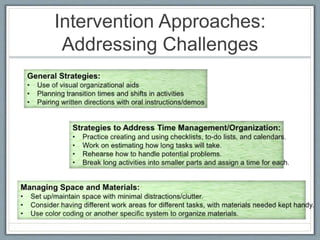
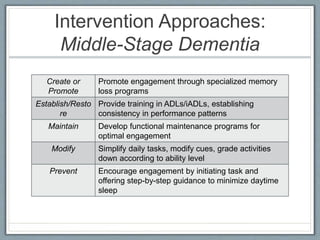
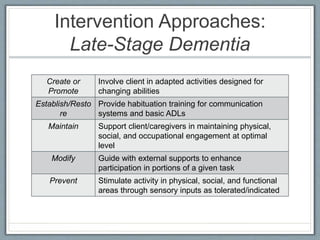
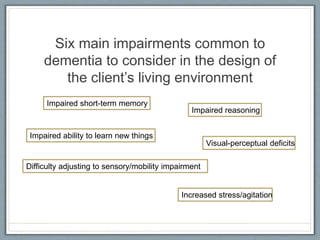
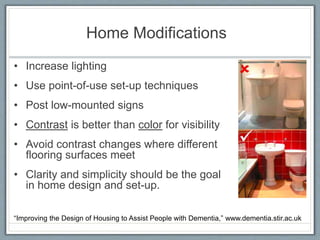
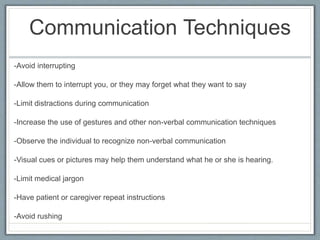
This document discusses dementia and Alzheimer's disease. It defines dementia as a general decline in mental abilities severe enough to interfere with daily life. Alzheimer's disease is the most common type of dementia, accounting for about two-thirds of cases. The document describes the signs and symptoms of Alzheimer's disease and how it progresses through early, middle, and late stages. It also discusses other types of dementia, like vascular dementia, as well as factors that can impact individuals with dementia like sundowning. Occupational therapy evaluation and intervention strategies are overviewed to maximize quality of life and engagement for individuals with dementia.