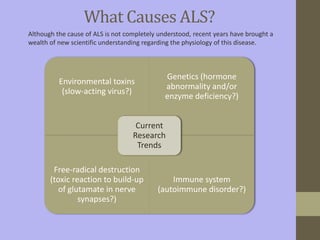
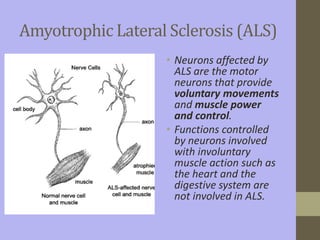
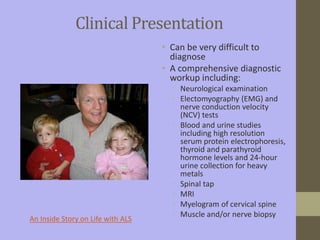
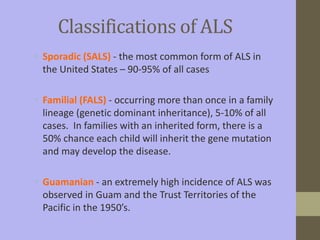
The document discusses Amyotrophic Lateral Sclerosis (ALS), also known as Lou Gehrig's disease, including causes, symptoms, classifications, stages of progression, medical interventions, the role of occupational therapy in evaluation and treatment, and resources for patients. ALS is a progressive neurodegenerative disease that affects motor neurons in the brain and spinal cord, leading to weakness and atrophy of muscles. Occupational therapy focuses on maintaining functional abilities, mobility, and independence through energy conservation techniques, adaptive equipment, and addressing challenges with activities of daily living.