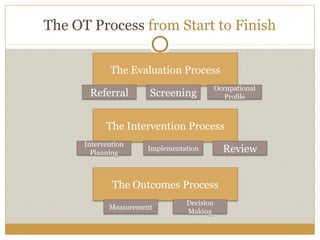
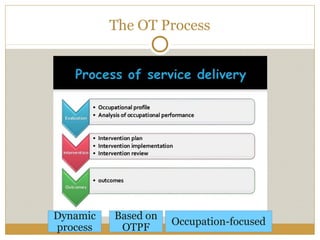
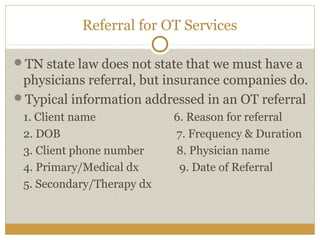
The OT process begins with a referral which leads to screening and evaluation to develop an occupational profile and plan of care. Intervention is implemented which focuses on occupation and graded challenges. Reevaluation assesses progress towards goals which informs outcomes of continuing, modifying, or discharging the client. Throughout the process, documentation in a SOAP note format is required for legal, ethical, and reimbursement purposes. The dynamic OT process is client-centered and based on enabling occupation.