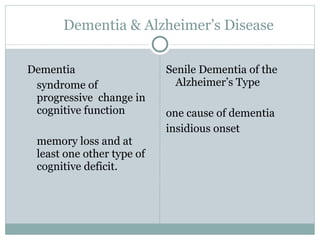
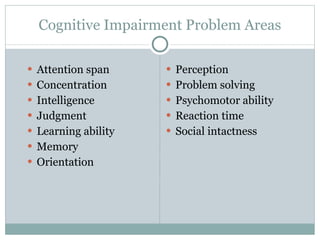
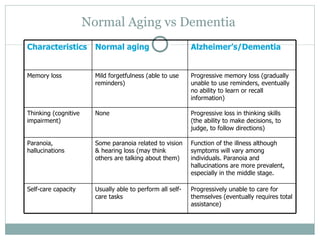
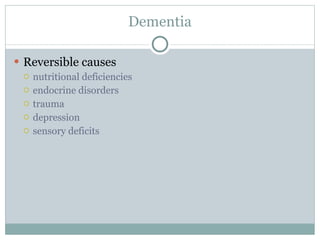
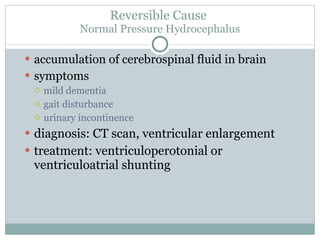
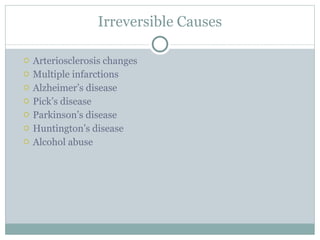
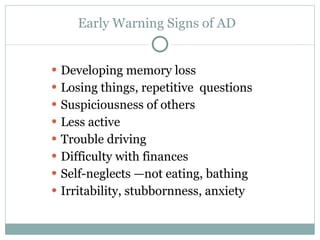
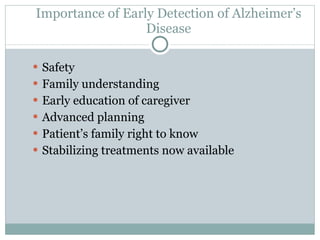
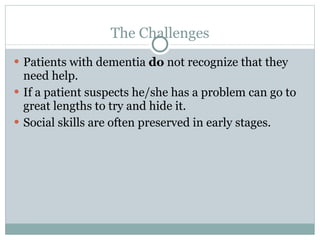
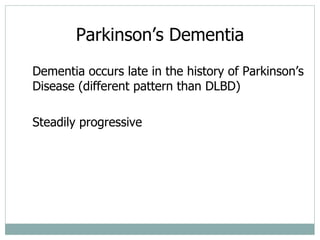
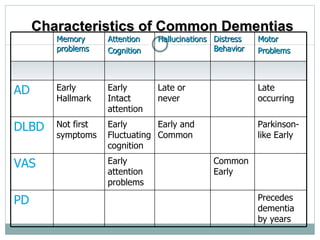
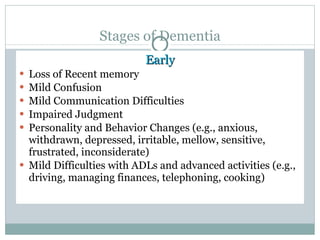
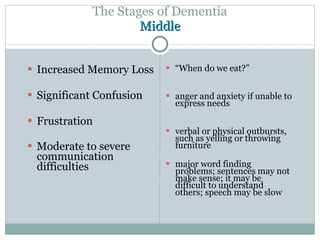
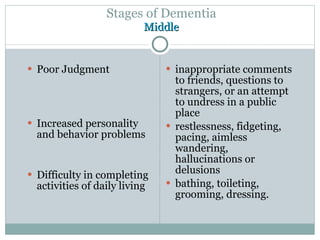
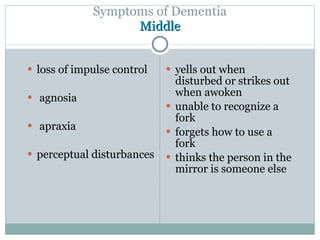
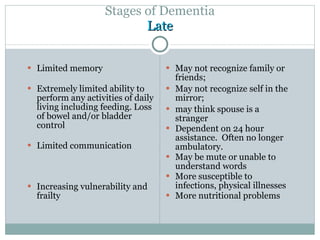
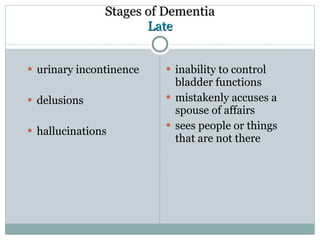
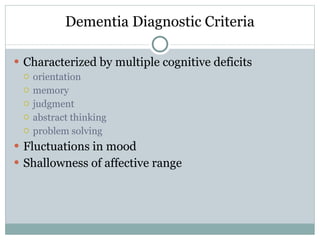
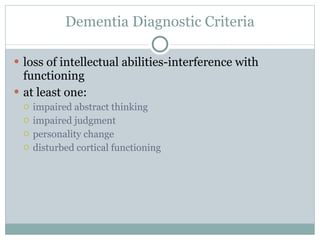
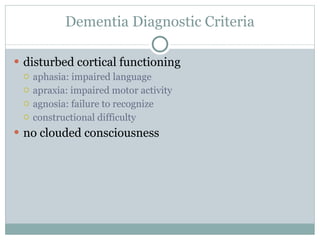
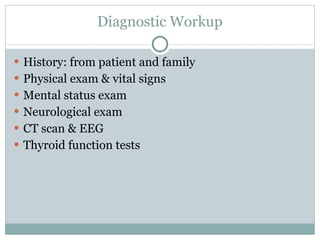
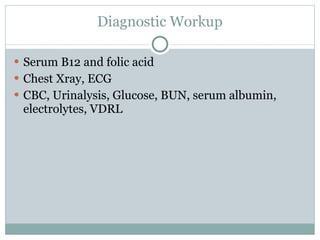
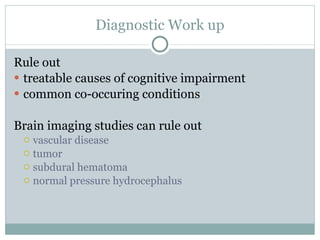
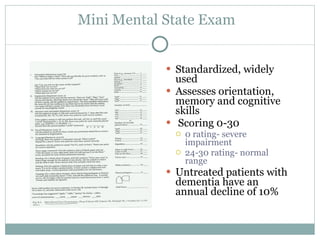
Dementia is a progressive decline in cognitive function including memory loss and at least one other cognitive deficit. Alzheimer's disease is the most common cause of dementia, characterized by plaques and tangles in the brain. Symptoms start with memory problems and gradually worsen to include problems with language, orientation, judgment, and ability to perform daily tasks. Dementia progresses through mild, moderate, and severe stages with increasing impairment. It can be caused by reversible or irreversible factors and is diagnosed through cognitive assessments and medical tests.