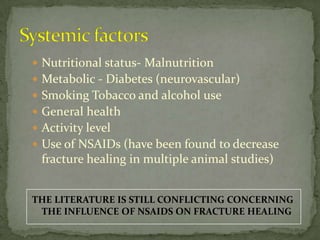
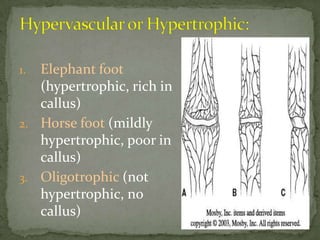
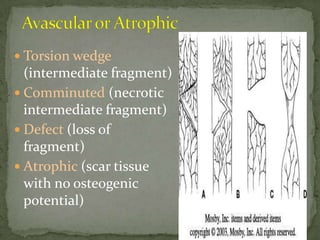
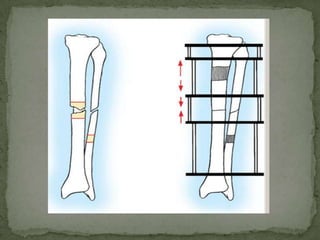
Approximately 5% of fractures result in non-unions and more in delayed unions. A delayed union occurs when healing is slower than average, between 3-6 months. Non-union is defined as no healing after 9 months. Factors contributing to delayed or non-union include systemic factors like nutrition, smoking, and local factors like soft tissue injury and fracture characteristics. Treatment involves addressing factors preventing healing, stabilizing the bone, bone grafting, and in some cases electrical or ultrasound stimulation to promote healing. Surgical techniques depend on the type and severity of the non-union.