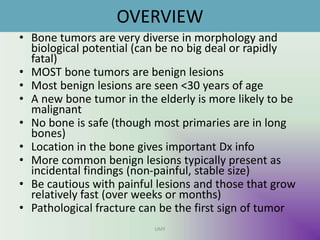
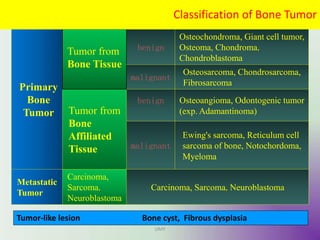
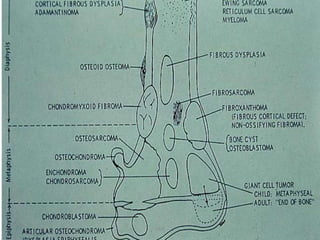
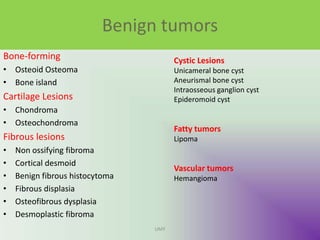
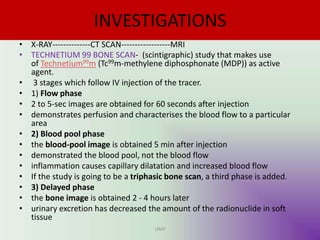
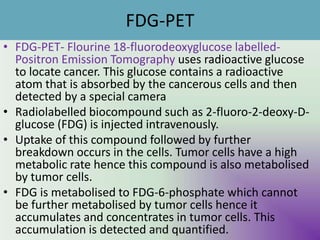
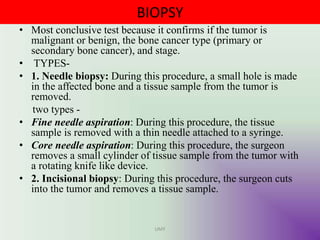
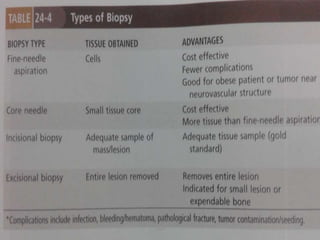
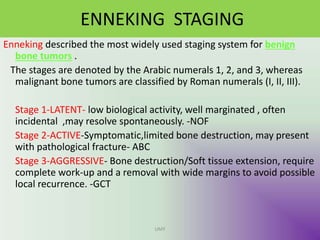
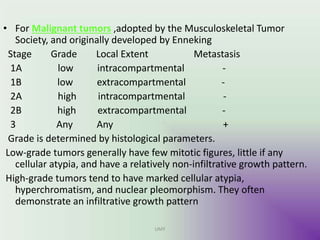
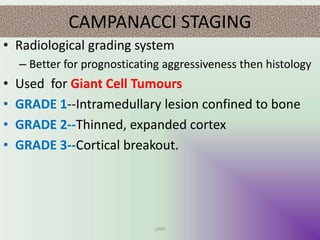
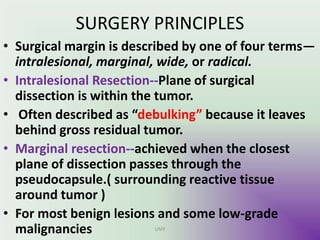
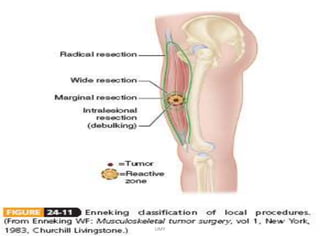
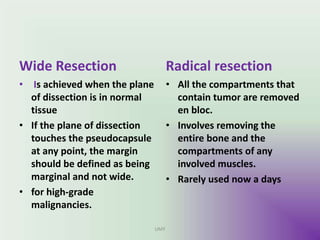
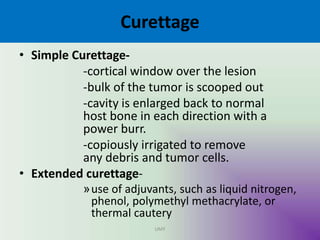
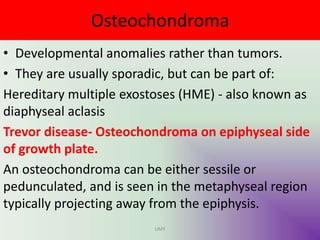
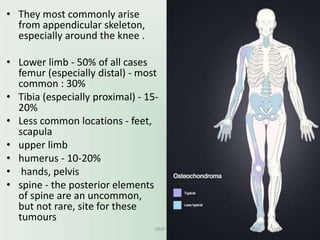
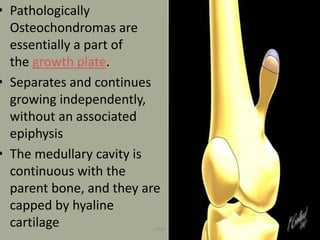
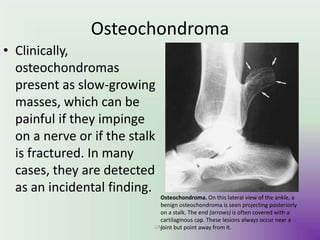
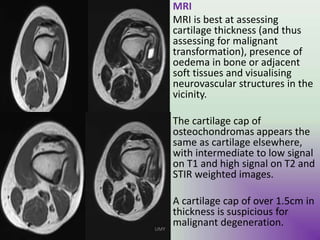
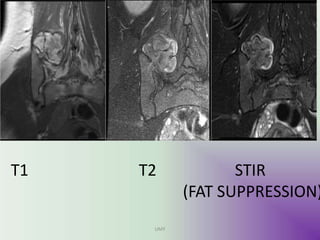
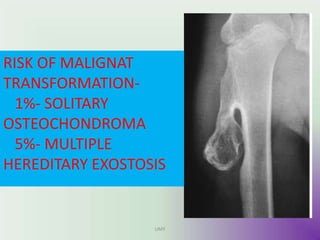
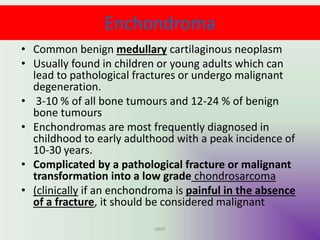
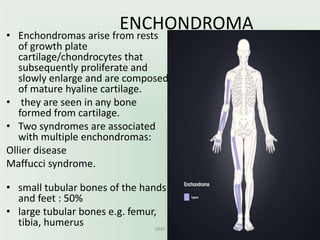
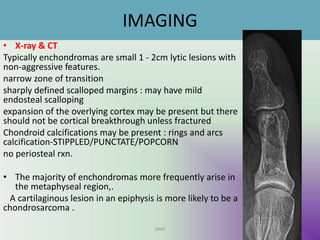
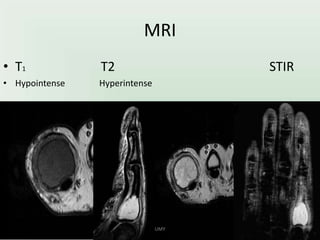
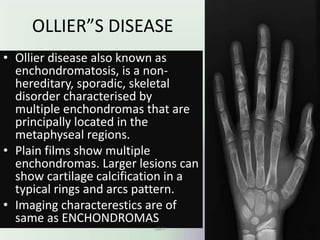
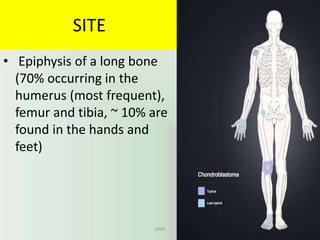
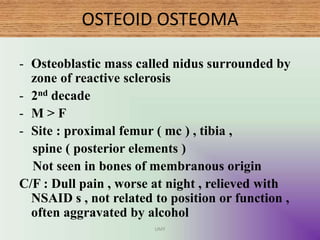
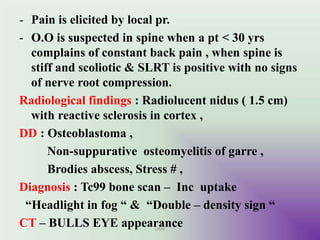
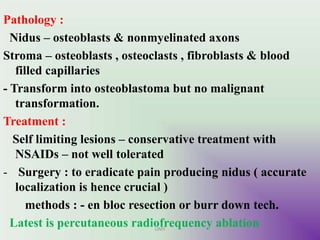
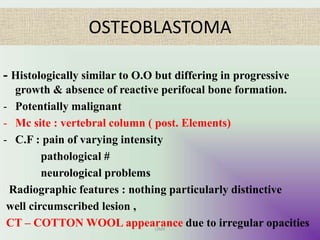
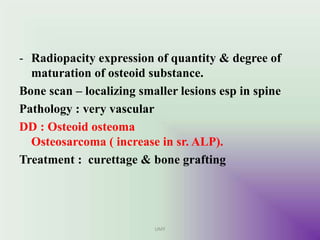
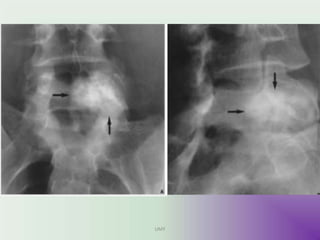
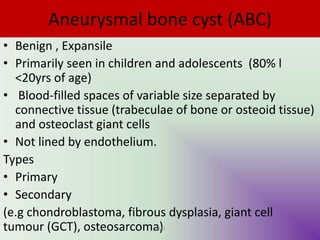
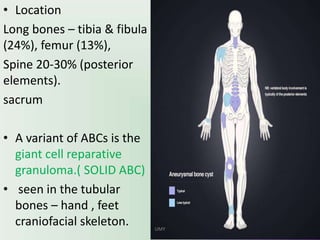
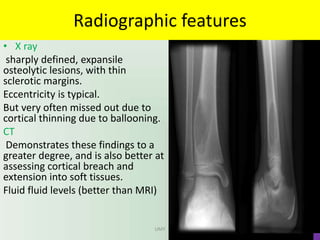
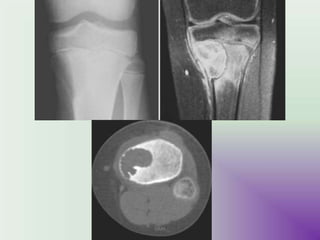
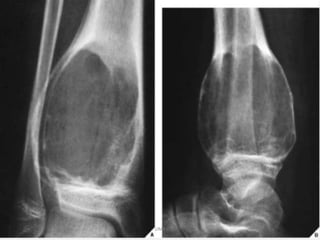
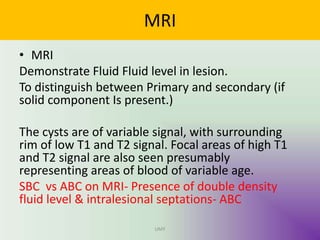
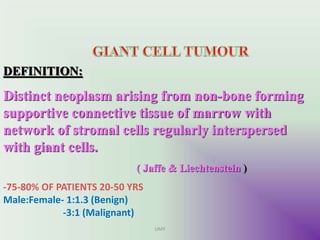
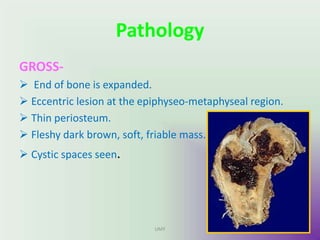
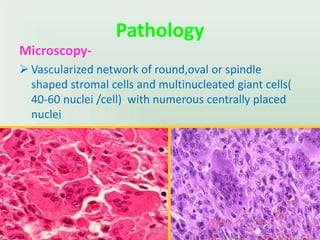
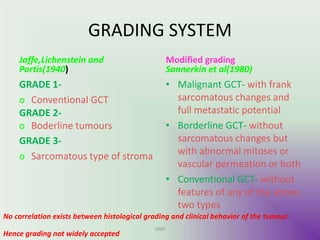
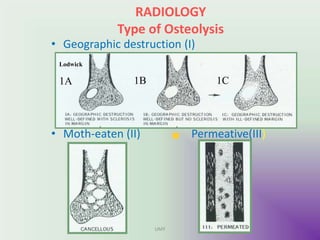
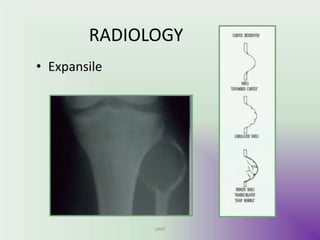
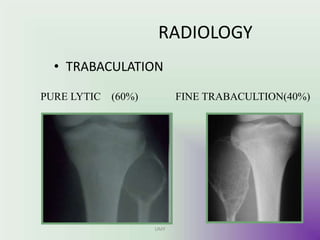
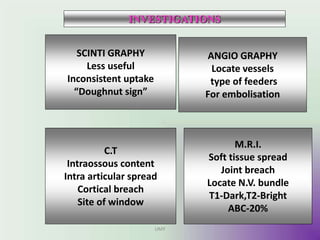
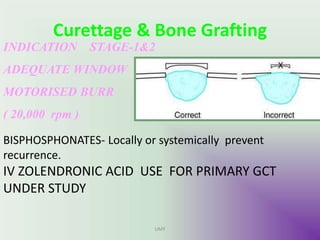
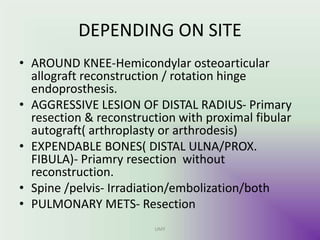
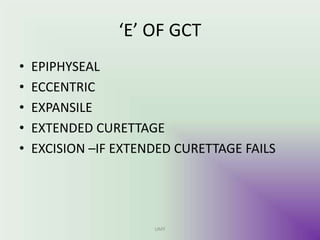
The document provides an overview of bone tumors, highlighting the distinction between benign and malignant types, their characteristics, and the typical demographic affected. It discusses various diagnostic methods including radiology, biopsy, and staging systems like Enneking and Campanacci to assess the tumors' aggressiveness and treatment options. Specific benign tumors such as osteochondroma and enchondroma, along with their imaging findings and clinical features, are also detailed.