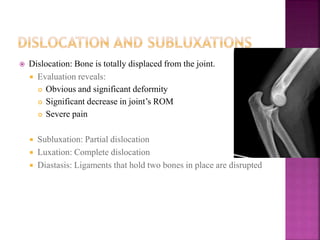
Trauma refers to physical injury caused by transfer of kinetic energy. A standardized protocol called Advanced Trauma Life Support (ATLS) exists for evaluating and treating trauma patients. It involves primary, secondary, and tertiary surveys to address life threats and identify injuries in a systematic manner. Common musculoskeletal injuries include fractures, dislocations, amputations, and soft tissue injuries. Proper splinting and hemorrhage control are important initial steps in management.