1. A 60-year-old man presented with worsening back pain for one month without any history of trauma.
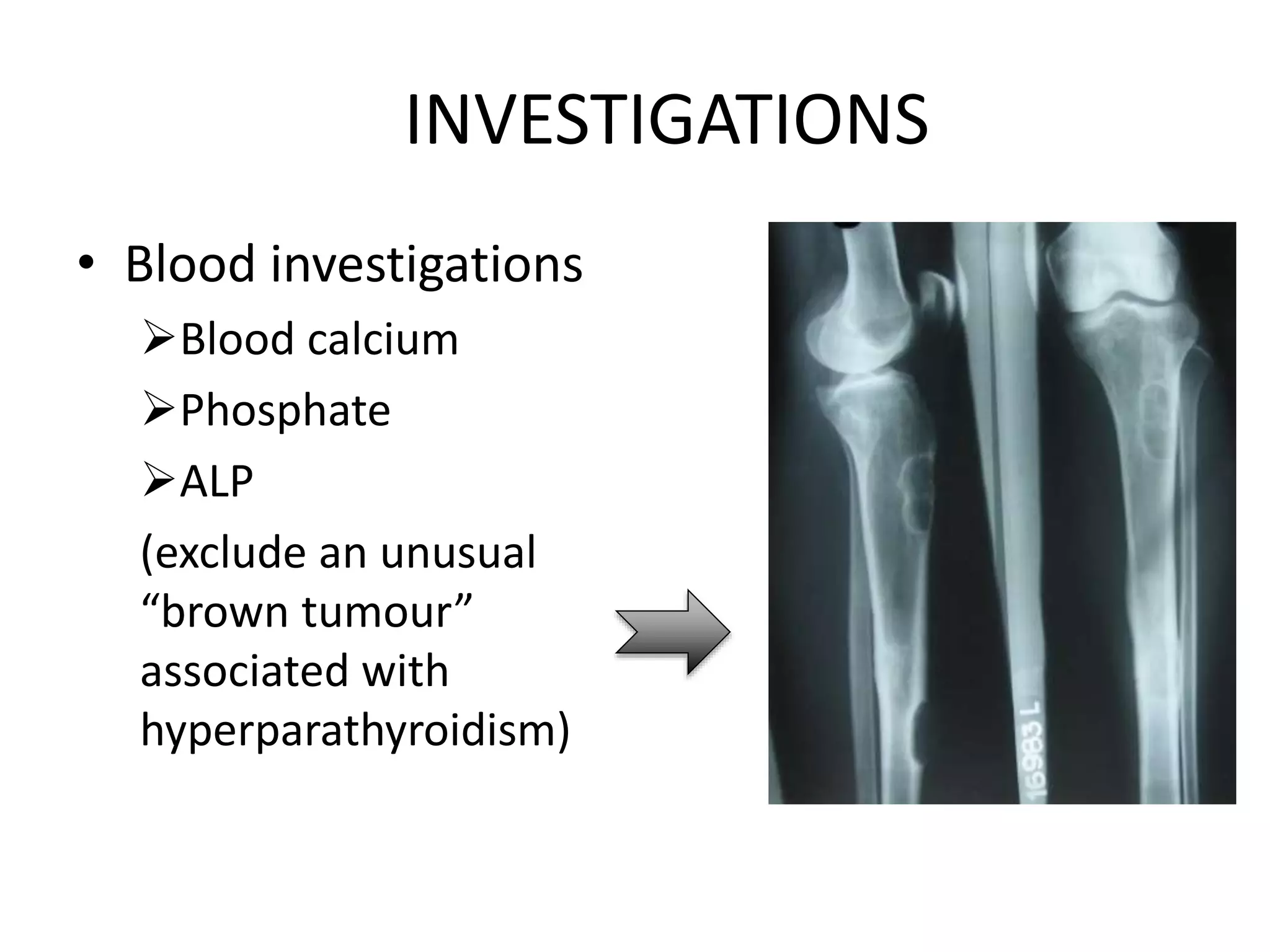
2. Blood tests showed a monoclonal gammopathy and elevated ESR of 100mm.
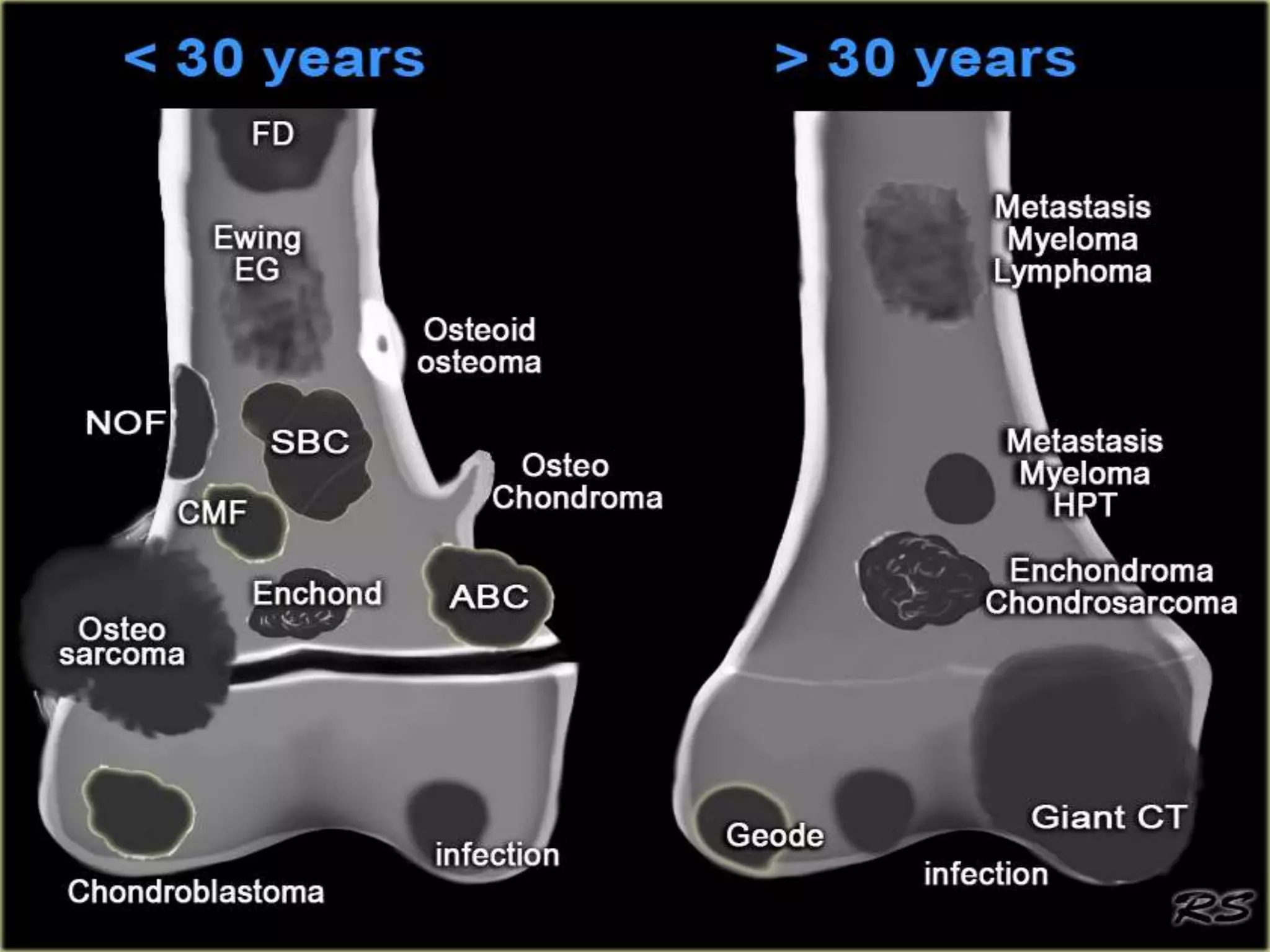
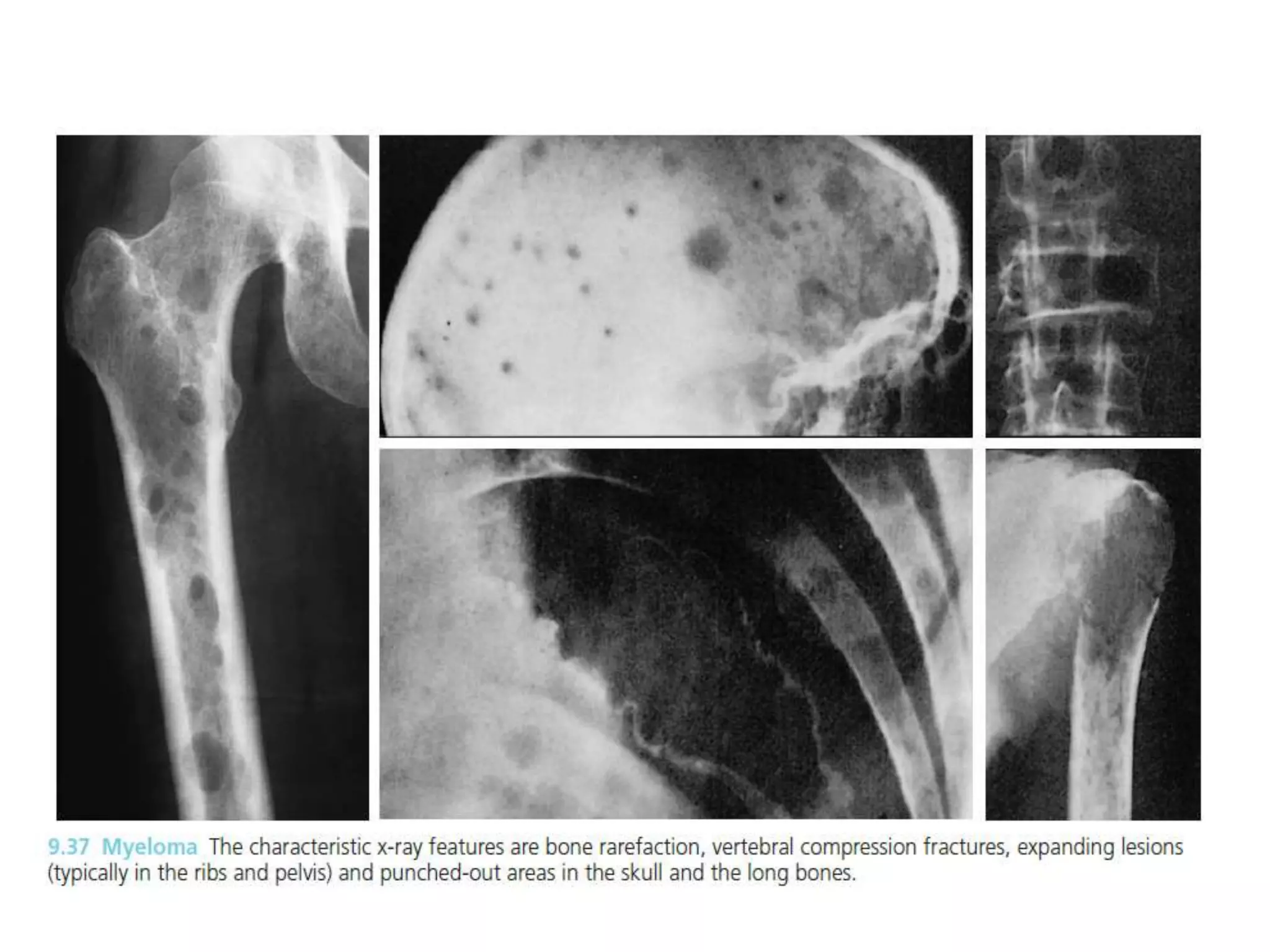
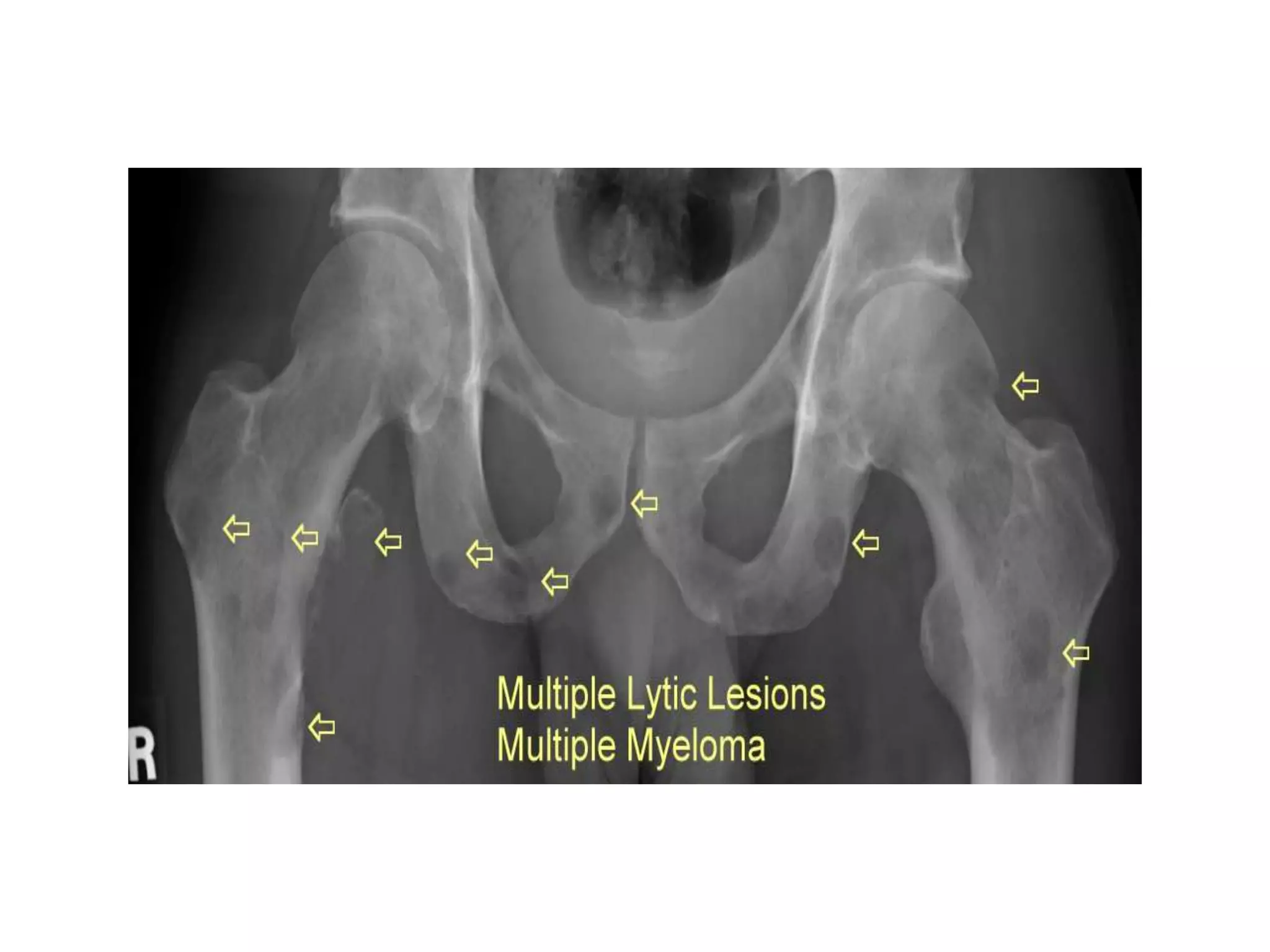
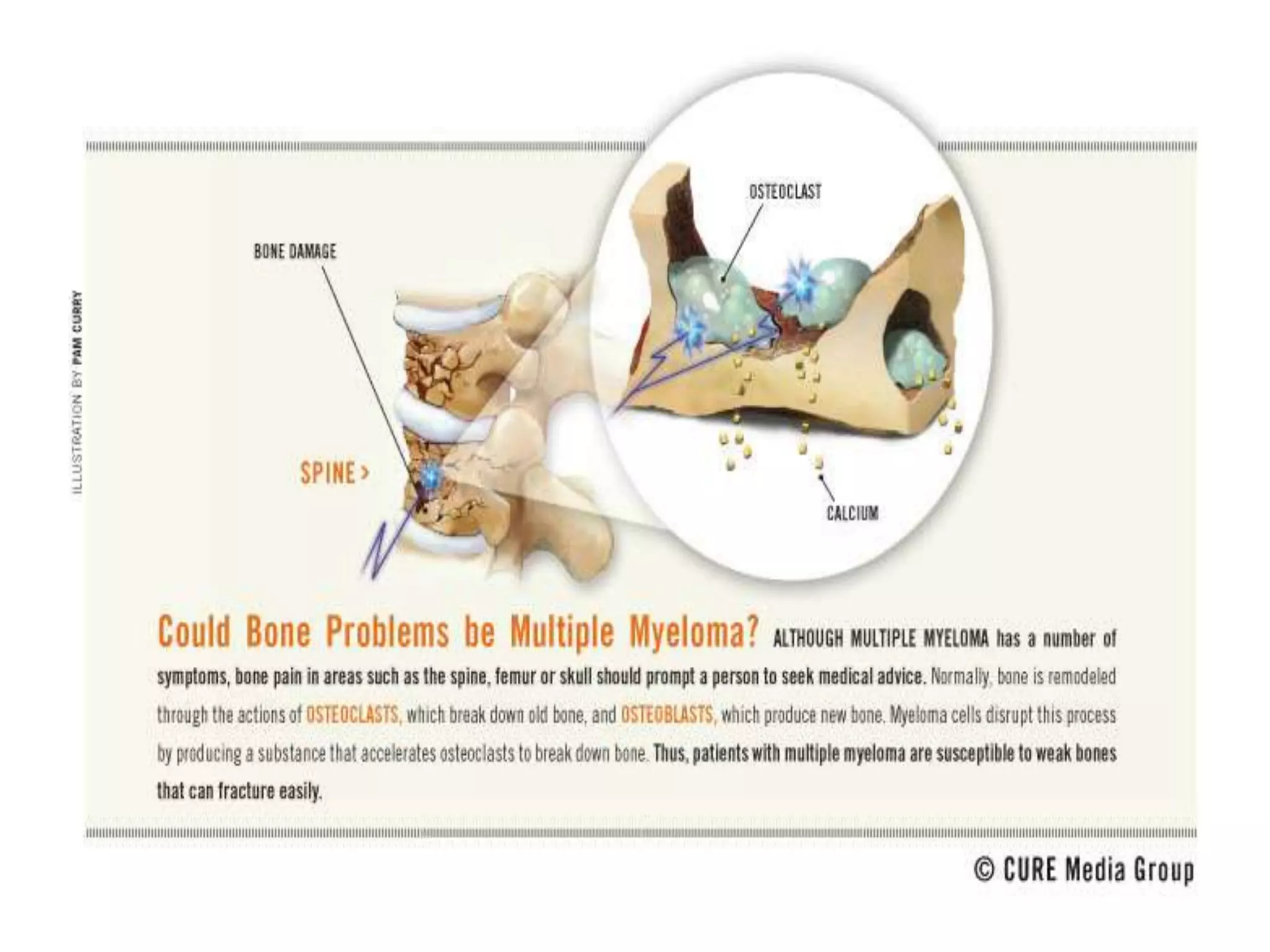
3. The main differential diagnosis is multiple myeloma, which commonly affects patients around age 45-65 and presents with bone pain due to lytic bone lesions caused by plasma cell infiltration and monoclonal protein production. Further investigations such as skeletal survey, serum and urine protein electrophoresis, and bone marrow biopsy are needed to confirm the diagnosis.